In our previous blog we wondered if some commentators, who have co-occurring disorders may be puzzled at how having a “spiritual malady” could be related in any way to have a co-occurring condition?
This is a pretty valid question?
In fact this may be at the heart of the issue in many cases of feeling the need to take medication for so-called co-occurring conditions?
Seeing alcoholism as partly the product of a spiritual malady, instead of the affective disorder I believe it to be, may influence certain AAs to seek additional help for supposed additional conditions when the manifestation of these conditions may actually be part of the emotional disorder of alcoholism?
It is at least worth considering?
For me sometimes there is a confusion with what is perceived to be a spiritual malady?
I do not believe I have the same type of spiritual malady as my wife for example who is an normie, earthling, normal person (whatever that is?) I believe, if any thing I have a super enhanced, at times turbo-charged, spiritual malady, often fuelled by stress/distress, as the result of my alcoholism.
I do not believe I have the same spiritual malady as other normal people such as those people who were in the Oxford Group.

That is not to say that normal people cannot be full of sin – a cursory look around the work and it’s events will soon confirm this is the case. What I am saying is that they do not have the emotion dysregulation or fear based responding that I seem to have which often prompts “sin”.
By sin I mean negative emotions that cause distress to me and others.
For example, false pride, intolerance, impatience, arrogance, shame, lust, gluttony, greed. Yes these all create distress.
The spiritual principles of AA and the 12 steps in particular were drawn from the 4 absolutes of the Oxford group, via initially the 6 steps and the idea of a spiritual malady is also borrowed from the Oxford group.
I have for several years wondered if the spiritual malady described in the Big Book adequate or accurate enough in describing what I suffer from.
I believe others have difficulties in reconciling the spiritual malady of the Big Book with their own alcoholism, addiction and co-occurring conditions?
Part of the problem may lie in not being specific enough about what alcoholism is.
It may be that research and the world have not progressed far enough to give a comprehensive account of what alcoholism is. Also the spiritual malady concept of AA has for 80 years helped millions of people recover from this most profound of conditions? So why change it if it’s not broke?
That is a good point? I am not advocating changing anything, I hope AA recovery remains as it is for 80 more years and much more years. I would not change one word in the first 164 pages of the BB.
However, many AAs ignore the spiritual malady thing completely, or do not do the steps, so, in my opinion, they often do not properly understand what they suffer from?
The magic of the the steps is that they seem to reveal the patterns of behaviour that our actions have prompted over the course of our lives. Maladaptive behaviours I should add. It helps us see ourselves and our condition of alcoholism and how it effects us and others.
It shows the areas of behaviour and attitudes that can be treated by working the steps. It shows us how our approach to life can possibly be transformed for the better.
For me personally it often showed a pattern of emotional responding to events that do not go my way!!?

As Bill Wilson once wrote we suffer when we cannot not get what we want or others seem to prevent us getting what we want.
My inventory of steps 4/5 showed me that my long lists of resentments were mainly the product of emotional immaturity and responding in an immature manner to not getting my way.
My inventory showed me also that I did not seem to have the facility previously to emotionally respond to the world in a mature way. As the world dominated me.
My recovery has thus since been about “growing up” a bit, however unsuccessful I am in this pursuit on occasion.
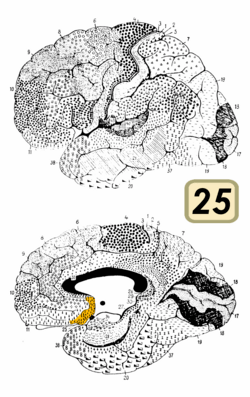
I have often written that this inherent emotional immaturity may even be linked to the possibility that the areas of my brain that regulate emotions have not matured properly as alcoholic seem to have different connectivity, functionality and morphology (size/volume) in this emotion regulation circuit/network to healthy normal people.
Alcoholics seem not to be able to fully process emotional information externally, i.e reading emotion expression of faces accurately, or internally reading what emotions we are having, or even whether we are hungry or tired!
So we have issues with emotions and somatic/body feeling states. This is perhaps compounded by most of us having experienced abuse or maltreatment which can also lead to alexithymic characteristics such as not being able to label or describe, verbally, emotional states we are experiencing – although we can be good at intellectualising these emotions – which is not the same as processing them.
Alcoholics and children of alcoholics have a tendency to avoid emotions (use avoidant coping strategies) in fact and to use emotional reasoning when arguing a point.
These emotion processing deficits also appear to make us more impulsive, and to choose lesser short term gain over greater long term gain in decision making. It can lead to a distress feeling state that can make us fear based, perfectionist, have catastrophic thoughts, intolerance of uncertainty, low frustration and distress tolerance, be reactionary, moody, and immature in our emotional responding.
But how has any of this got anything to do with the so-called spiritual malady we are suppose to suffer from?
I believe the spiritual malady mixed with the ancedotal evidence throughout the BiG Book hints at these emotional difficulties as being an intrinsic part of our alcoholism, “We were having trouble with personal relationships, we couldn’t control our emotional natures, we were a prey to misery and depression, we couldn’t make a living, we had a feeling of uselessness, we were full of fear, we were unhappy…”
It was 80 years ago, so our knowledge base has moved on greatly from when the Big Book was written. Hence I believe we should appreciate that this definition of our condition has been updated by research into emotions especially in the last 20 years.
I am happy to say a spiritual malady is what we suffer from, as the steps provide a solution to my emotion disorder by treating it as a spiritual malady but I do not think it is the straightforward spiritual malady adopted by AA from the Oxford Group, mainly because in the majority of situations I do not choose to sin, the sinning seems to happen to me. In other words it is the consequence of my fear based condition, this affective disorder.
The Oxford Group explain a general spiritual malady that all people can have. I do not think alcoholics are like all people. We are human beings, but extreme versions of human beings. I believe, even when I try my best to be virtuous and holy, I could sin at the sinning Olympics for my country. I am that naturally good at it!
I sin so naturally, effortlessly and usually without even trying. I believe my so-called defects of character are linked to my underlying emotional disorder of alcoholism.
Sins I believe are the poisoned fruit of fear, often helped along in alcoholics by false pride, shame and guilt. These defects are related to me being an alcoholic, they are intrinsic to my condition.
In order to illustrate how I believe my spiritual malady is the consequence of my emotional disorder, called alcoholism/addiction first let’s go back to where this idea of spiritual malady came from.
According to a wonderful pamphlet “What is the Oxford Group” written by The Layman With a Notebook ” Sin can kill not only the soul but mind, talents, and happiness as surely as a malignant physical disease can kill the body…
Sin is a disease with consequences we cannot foretell or judge; it is as contagious as any contagious disease our bodies may suffer from. The sin we commit within this hour may have unforeseen dire consequences even after we have long ceased to draw living breath…
…Like physical disease Sin needs antiseptics to prevent it from spreading; the soul needs cleaning as much as the body needs it…
Unhappiness to us and others, discontent, and, frequently, mental and bodily ill health are the direct results of Sin.
…Morbidity of mind must affect the physical health. If we can be absolutely truthful to ourselves we can analyse our sins for ourselves and trace their mental and physical effects. Sins can dominate us mentally and physically until we are their abject slaves. We cannot get rid of them by deciding to think no more about them; they never leave us of their own accord, and unless they are cut out by a decided surgical spiritual operation which will destroy them, roots and all, and set us free from their killing obsession, they grow in time like a deadly moss within us until we become warped in outlook not only towards others but towards ourselves….”
One can see how this concept of sin disease or in other words spiritual malady could be and was applied to early AA and incorporated into the Big Book of AA.
However, it is equally stating, I believe, that alcoholics suffer from the same spiritual malady as other people but our spiritual malady has led to chronic alcoholism, this is the manner in which sin has dominated “mentally and physically until we are their abject slaves”.
In fact the Big book’s first chapters look more at the manifestation of this malady, problem drinking, than the malady. It suggests that there is more than this malady, there is also a physical reason for alcoholism- an allergy (or abnormal reaction) to alcohol. So this is a departure from the Oxford Group as it clearly states that alcoholism is more than a spiritual malady. It is not simply the consequence of this spiritual malady although this malady may contribute. So is this saying some of us are spiritually ill while also having an abnormal reaction to alcohol?
In the foreword The Doctor’s Opinion suggests that “the body of the alcoholic is quite as abnormal as his mind.” and a first mention of a disorder more than “spiritual” is suggested, “It did not satisfy us to be told that we could not control our drinking just because we were maladjusted to life, that we were in full flight from reality, or were outright mental defectives. These things were true to some extent, in fact, to a considerable extent with some of us. (my emphasis)
“The doctor’s theory that we have an allergy to alcohol interests us…as ex-problem drinkers, we can say that his explanation makes good sense. It explains many things for which we cannot otherwise account.”
“the action of alcohol on these chronic alcoholics is a manifestation of an allergy; that the phenomenon of craving is limited to this class and never occurs in the average temperate drinker.”
Here we have an abnormal reaction to alcohol and for some alcoholics a maladjustment to life.
For me this maladjustment to life is not exactly the same as the spiritual disease mentioned in the Oxford Group pamphlet.
All of my academic research in the last 6 years has explored the possibility that this “maladjustment to life” is more than a spiritual malady, i.e. it is not simply the consequence of Sin but the result of abnormal responding, emotionally (which has obvious consequences for sinning) to life.
This emotion dysregulation, as I name it, has consequences for how we feel about ourselves, how we interact with people, how much we feel we belong, how rewarding alcohol and drugs are, how much these substances make us feel better about ourselves (fix our feelings ) and how they turn off the internal critic of maladaptive and negative self schemas.
In fact our first “spiritual” wakening was probably the result of drinking as it transformed how we felt about ourselves and the world in which we lived. I know it did for me. In fact, I felt “more me” when I drank, it was like I escaped a restrictive sense of self to be a more expansive, people loving self. I had a connection with the world I could not generate myself, when sober.
I was a “spirit awakening” if nothing else? It is interesting that a common definition of “spiritual” as it relates to AA, is a sense of connection with others.
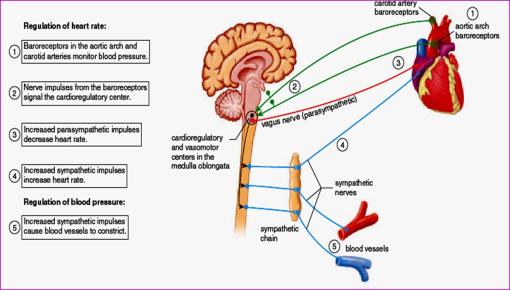
As the BB states “Men and women drink essentially because they like the effect produced by alcohol. The sensation is so elusive that, while they admit it is injurious, they cannot after a time differentiate the true from the false. To them, their alcoholic life seems the only normal one. They are restless, irritable and discontented, unless they can again experience the sense of ease and comfort which comes at once by taking a few drinks—”
For me this section is saying our emotion dysregulation leads to feelings of being “restless, irritable and discontented” which prompt a return to drinking.
The Doctor’s Opinion even offers some classifications of alcoholics “The classification of alcoholics seems most difficult, and in much detail is outside the scope of this book. There are, of course, the psychopaths who are emotionally unstable… the manic-depressive type, who is, perhaps, the least understood by his friends, and about whom a whole chapter could be written.”
This section would appear to be stating clearly that there alcoholics who have other (co-occurring) conditions or conditions appearing as co-occurring?
I contend that alcoholism is an emotional disorder which results in chemical dependency on the substance of alcohol. However in order to treat it we have to first contend with the symptomatic manifestation of this disorder, chronic alcohol use, as it is the most life threatening aspect of this disorder when we present our selves at AA.
What we used once to regulate negative emotions and a sense of self has eventually come to regulate our emotions to such an extent that any distress leads to the compulsive response of drinking. Alcoholics had become a compulsive disorder to relief distress not to induce pleasure.
The “spiritual malady” of the Oxford group seems enhanced in me, I believe I sin more than normal people because of my emotional immaturity and reactivity. My “loss of control” over drinking is also linked to emotion processing difficulties as it prompted impulsive, uninhibited drinking.
This emotional immaturity is referenced throughout the Big Book I believe.
“… He begins to think life doesn’t treat him right. He decides to exert himself more. He becomes, on the next occasion, still more demanding or gracious, as the case may be. Still the play does not suit him. Admitting he may be somewhat at fault, he is sure that other people are more to blame. He becomes angry, indignant, self-pitying. ”
“Whatever our protestations, are not most of us concerned with ourselves, our resentments, or our self-pity? Selfishness—self-centeredness! That, we think, is the root of our troubles. Driven by a hundred forms of fear, self-delusion, self-seeking, and self-pity, we step on the toes of our fellows and they retaliate. ”
“So our troubles, we think, are basically of our own making. They arise out of ourselves…”
“…Our liquor was but a symptom…”
“Resentment is the ”number one“ offender. It destroys more alcoholics than anything else. From it stem all forms of spiritual disease, for we have been not only mentally and physically ill, we have been spiritually sick.”
For me this is saying that out of my emotion dysregulation “stem all forms of spiritual disease”.
It then talks of the fear that “was an evil and corroding thread; the fabric of our existence was shot through with it. ”
The list of emotional difficulties continues throughout the Big book’s first 164 pages.
One of the earliest studies on AA members concluded that they were linked in commonality by two variables, emotional immaturity and grandiosity! I would contend that grandiosity is a part of emotional immaturity. I also contend that our “maladjustment to life” is based on emotional immaturity which is in itself a function of emotion regulation and processing deficits.
A book titled Matt Talbot by Morgan Costelloe has cites this reference – “American authorities on alcoholism hold that the following psychological traits are commonly found in alcoholics:
> 1. A high level of anxiety in interpersonal relations
> 2. Emotional immaturity
> 3. Ambivalence towards authority
> 4. Low frustration tolerance
> 5. Low self-esteem
> 6. Perfectionism
> 7. Guilt
> 8. Feelings of isolation”
The list is almost word-for-word identical with one in Howard Clinebell’s
“Understanding and Counseling the Alcoholic” p 53 of the revised edition of 1968 (the original edition appeared in 1956), the only difference being that Clinebell included grandiosity and compulsiveness.
Years after the Big Book Bill Wilson wrote about this emotion immaturity in the guise of discussing emotional sobriety, for me what he is saying that our emotional difficulties are present in long term recovery and need to be addressed – in other words there is more to alcoholism than sinning and drinking. What we are left with after the steps is ongoing and underlying difficulties with living life on life’s terms because we are emotionally immature. This I believe also preceded our drinking, for many of us anyway?
For many recovering alcoholics this may be another unpalatable truth, that they have issues with emotional responding, with being emotionally mature. If further validation is required I suggest a frank conversation with a loved one, wife, husband, child, parent, etc.
Here is what Bill Wilson wrote ” Those adolescent urges that so many of us have for top approval, perfect security, and perfect romance—urges quite appropriate to age seventeen—prove to be an impossible way of life when we are at age forty-seven or fifty-seven. Since AA began, I’ve taken immense wallops in all these areas because of my failure to grow up, emotionally and spiritually”. (my emphasis)
Bill continues “Suddenly I realized what the matter was. My basic flaw had always been dependence – almost absolute dependence – on people or circumstances to supply me with prestige, security, and the like. Failing to get these things according to my perfectionist dreams and specifications, I had fought for them. And when defeat came, so did my depression.”
” Emotional and instinctual satisfactions, I saw, were really the extra dividends of having love, offering love, and expressing a love appropriate to each relation of life… I was victimized by false dependencies… For my dependency meant demand—a demand for the possession and control of the people and the conditions surrounding me.”
For me this is emotional immaturity, regulating ones emotions and distress via external dependencies on others, demanding in an immature manner that others do one’s bidding?
I would suggest in relation to the issue of co-morbidities that one try to deal with these alcoholism related issues and then see if there are any other to deal with afterwards. For me, as someone who has been treated for anxiety and depression prior to recovery the 12 steps appear to have treated these as emotional consequences of my underlying condition of emotion dysregulation which I call alcoholism.

I think part of the issue is whether doctors, who know in my experience often know next to nothing generally about alcoholism, can always properly diagnose depression and anxiety in someone suffering from alcoholism?
I also think the issues are complicate because alcoholism have some many similarities to GAD, MDD, OCD, and so on. They all may be similar but different.
This is why we need a satisfactory definition of what alcoholism and addition is? Rather than describing these conditions in terms of the manifest symptoms, i.e chronic substance abuse or, at times, vague “spiritual maladies”.
For example, one variable I believe is slightly different in alcoholism to other affective disorders is distress based impulsivity which leads to maladaptive decision making, it leads to always wanting more of that…that anything.
These may be specific to addictive behaviours.
It may also be that we feel we have a co-occurring disorder because the underlying distress states prompt similar reactions in various differing disorders.
My distress feeds perfectionism, and catastrophic thinking as with other anxiety disorders like OCD, does that mean I have OCD too?
Maybe or maybe not? My tendency to not regulate emotions has caused a distress state since childhood, it feeds into perfectionism and many other manifestations like always wanting just one more…?
It is the always wanting one more that makes my affective disorder that of addiction and not another disorder.
My affective disorder via various neural and cognitive – affective mechanisms leads to chronic substance use and dependency of these substances.
GAD, MDD, OCD have different manifestations and different mechanisms.
If we start by trying to recover from alcoholism and addiction and find we still have other issues then obviously address these with outside professional and specialist help.
I believe we can unwittingly complicate our treatment of alcoholism by believing we have (and treating) other conditions we see as distinct from alcoholism but which are in fact part of this condition called alcoholism.
I never fully knew what alcoholsim was until I did the 12 steps. Only then did it become clear what I suffered from?
I have suggested clearly in previous blogs how I think AA’s 12 recovery programme helps specifically with problems of emotion dysregulation.
How the Alcoholics Anonymous-12-step-program of recovery helps with emotional dysregulation
Maintaining Emotional Sobriety (and sanity) via the steps 10-12.
These illustrate how the 12 step programme can help with an emotion dysregulation disorder.

I end, however, with some words from a doctor who seems to be suggesting that AA works because it makes us more emotionally healthy. For me she is saying how AA treats emotional illness.
An article by Dr. Jacqueline Chang’s paper given to the National Workshop for Health Liaison in York in 1998 and published in the Winter 1999 edition of the AA News suggests that
“The principles of the programme of Alcoholics Anonymous are scientific and closely follow all the helping therapies which lead people to emotional well-being.
AA proposes living “ One Day at a Time”. It is emotionally healthy to live in the day … in the here and now. Professional therapists teach people to live in the present. AA encourages members to share their experience, strength and hope with other members. It is emotionally healthy to accept our past experiences, however painful, as past events and move on to a richer, more fulfilling future.
Step 1 in the AA programme is “ We admitted we were powerless over alcohol – that our lives had become unmanageable”. It is emotionally healthy to surrender and accept things over which we have no control.
“God grant us the serenity to accept the things we cannot change, courage to change the things we can and the wisdom to know the difference” is the Serenity Prayer used at every AA meeting. It is emotionally healthy to prioritise problems. The Serenity Prayer is the greatest exercise in prioritisation.
It is emotionally healthy to accept that we cannot change a particular situation but we can change the way we react to it.
It is emotionally healthy to accept yourself as you are.
It is emotionally healthy to recognise your environment and interact with it as it is, not as you wish it would be. It is emotionally healthy to associate or be in contact with other human beings.
It is emotionally healthy to be altruistic – to help others without question or expectation.
It is emotionally healthy to anticipate – to plan for future discomfort or crises. This is the function of the AA Step programme. ”
AA provides many ways of becoming more emotionally well, which ultimately means more emotionally mature.