Impulsivity or lack of behaviour inhibition, especially when distressed, is one psychological mechanisms which is implicated in all addictive behaviour from substance addiction to behaviour addiction.
It is, in my view, linked to the impaired emotion processing as I have elucidated upon in various blogs on this site.
This impulsivity is present for example in those vulnerable to later alcoholism, i.e. sons and daughters of alcoholic parents or children from a family that has a relatively high or concentrated density of alcoholics in the family history, right through to old timers, people who have decades of recovery from alcoholism.
It is an ever present and as a result part of a pathomechanism of alcoholism, that is it is fundamental to driving alcoholism to it’s chronic endpoint.
It partly drives addiction via it’s impact on decision making – research shows people of varying addictive behaviours choose now over later, even if it is a smaller short term gain over a greater long term gain. We seem to react to relieve a distress signal in the brain rather than in response to considering and evaluating the long term consequences of a decision or act.
No doubt this improves in recovery as it has with me. Nonetheless, this tendency for rash action with limited consideration of long term consequence is clearly a part of the addictive profile. Not only do we choose now over then, we appear to have an intolerance of uncertainty, which means we have difficulties coping with uncertain outcomes. In other words we struggle with things in the future particularly if they are worrying or concerning things, like a day in court etc. The future can continually intrude into the present. A thought becomes a near certain action, again similar to the though-action fusion of obsessive compulsive disorder. It is as if the thought and possible future action are almost fused, as if they are happening in unison.
Although simple, less worrying events can also make me struggle with leaving the future to the future instead of endless and fruitlessly ruminating about it in the now. In early recovery especially I found that I had real difficulty dealing with the uncertainty of future events and always thought they would turn out bad. It is akin to catastrophic thinking.
If a thought of a drink entered into my head it was so distressing, almost as if I was being dragged by some invisible magnet to the nearest bar. It was horrendous. Fortunately I created my own thought action fusion to oppose this.
Any time I felt this distressing lure of the bar like some unavoidable siren call of alcohol I would turn that thought into the action of ringing my sponsor. This is why sponsees should ring sponsors about whatever, whenever in order to habitualize these responses to counteract the automatic responses of the addicted brain.
I think it is again based on an inherent emotion dysregulation. Obsessive thoughts are linked to emotion dysregulation.
My emotions can still sometimes control me and not the other way around.
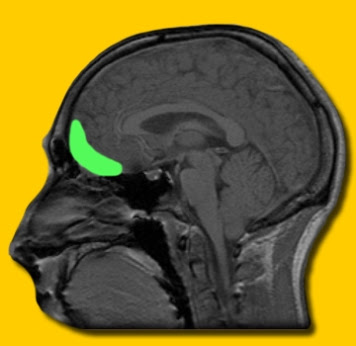
Apparently we need to recruit the frontal part of the brain to regulate these emotions and this is the area most damaged by chronic alcohol consumption.
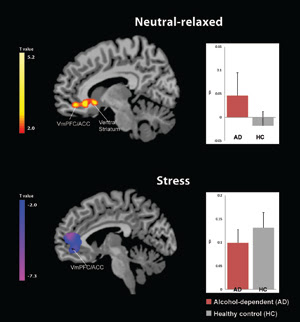
As a result we find it difficult to recruit this brain area which not only helps regulate emotion but is instrumental in making reflective, evaluative decisions about future, more long term consequence. As a result addicts of all types appear to use a “bottom up” sub-cortical part of the brain centred on the amgydala region to make responses to decisions instead of a “top down” more cortical part of the brain to make evaluative decisions.
We thus react, and rashly act to relieve the distress of undifferentiated emotions, the result of unprocessed emotion rather than using processed emotions to recruit the more cortical parts of the brain.
Who would have though emotions were so instrumental in us making decisions? Two parts of the brain that hold emotions in check so that they can be used to serve goal directed behaviour are the orbitofrontal cortex and the ventromedial prefrontal cortex.
These areas also keep amgydaloid responding in check. Unfortunately these two areas are impaired in alcoholics and other addictive behaviours so their influence on and regulation of the amgydala is also impaired.
This means the sub cortical areas of the amgydala and related regions are over active and prompt not a goal directed response to decision making but a “fight or flight” response to alleviate distress and not facilitate goal directed behaviour.
Sorry for so much detail. I have read so much about medication recently which does this or that to reduce craving or to control drinking but what about the underlying conditions of alcoholism and addictive behaviour? These are rarely mentioned or considered at all.
We always in recovery have to deal with alcoholism not just it’s symptomatic manifestation of that which is chronic alcohol consumption. This is a relatively simple point and observation that somehow alludes academics, researchers and so-called commentators on this fascinating subject.
Anyway that is some background to this study which demonstrates that long term AA membership can reduce this impulsivity and perhaps adds validity to the above arguments that improved behaviour inhibition and reducing impulsivity is a very possible mechanism of change brought about by AA membership and the 12 step recovery program.
It shows how we can learn about a pathology from the recovery from it!
Indeed when one looks back at one’s step 4 and 5 how many times was this distress based impulsivity the real reason for “stepping on the toes of others” and for their retaliation?
Were we not partly dominated by the world because we could not keep ourselves in check? Didn’t all our decisions get us to AA because they were inherently based on a decision making weakness? Isn’t this why it is always useful to have a sponsor, someone to discuss possible decisions with?
Weren’t we out of control, regardless of alcohol or substance or behaviour addiction? Isn’t this at the heart of our unmanageability?
I think we can all see how we still are effected by a tendency not to think things through and to act rashly.
The trouble it has caused is quite staggeringly really?
Again we cite a study (1) which has Rudolf H. Moos as a co-author. Moos has authored and co-authored a numbered of fine papers on the effectiveness of AA and is a rationale beacon in a sea of sometimes quite controversial and ignorant studies on AA, and alcoholism in general.
“Abstract
Reduced impulsivity is a novel, yet plausible, mechanism of change associated with the salutary effects of Alcoholics Anonymous (AA). Here, we review our work on links between AA attendance and reduced impulsivity using a 16-year prospective study of men and women with alcohol use disorders (AUD) who were initially untreated for their drinking problems. Across the study period, there were significant mean-level decreases in impulsivity, and longer AA duration was associated with reductions in impulsivity…
Among individuals with alcohol use disorders (AUD), Alcoholics Anonymous (AA) is linked to improved functioning across a number of domains [1, 2]. As the evidence for the effectiveness of AA has accumulated, so too have efforts to identify the mechanisms of change associated with participation in this mutual-help group [3]. To our knowledge, however, there have been no efforts to examine links between AA and reductions in impulsivity-a dimension of personality marked by deficits in self-control and self-regulation, and tendencies to take risks and respond to stimuli with minimal forethought.
In this article, we discuss the conceptual rationale for reduced impulsivity as a mechanism of change associated with AA, review our research on links between AA and reduced impulsivity, and discuss potential implications of the findings for future research on AA and, more broadly, interventions for individuals with AUD.
Impulsivity and related traits of disinhibition are core risk factors for AUD [5, 6]. In cross-sectional research, impulsivity is typically higher among individuals in AUD treatment than among those in the general population [7] and, in prospective studies, impulse control deficits tend to predate the onset of drinking problems [8–11]
Although traditionally viewed as static variables, contemporary research has revealed that traits such as impulsivity can change over time [17]. For example, traits related to impulsivity exhibit significant mean- and individual-level decreases over the lifespan [18], as do symptoms of personality disorders that include impulsivity as an essential feature [21, 22]. Moreover, entry into social roles that press for increased responsibility and self-control predict decreases in impulsivity [16, 23, 24]. Hence, individual levels of impulsivity can be modified by systematic changes in one’s life circumstances [25].
Substance use-focused mutual-help groups may promote such changes, given that they seek to bolster self-efficacy and coping skills aimed at controlling substance use, encourage members to be more structured in their daily lives, and target deficits in self-regulation [26]. Such “active ingredients” may curb the immediate self-gratification characteristic of disinhibition and provide the conceptual grounds to expect that AA participation can press for a reduction in impulsive inclinations.
…the idea of reduced impulsivity as a mechanism of change…it is consistent with contemporary definitions of recovery from substance use disorders that emphasize improved citizenship and global health [31], AA’s vision of recovery as a broad transformation of character [32], and efforts to explore individual differences in emotional and behavioral functioning as potential mechanisms of change (e.g., negative affect [33,34]).
Several findings are notable from our research on associations between AA attendance and reduced impulsivity. First, consistent with the idea of impulsivity as a dynamic construct [18, 19], mean-levels of impulsivity decreased significantly in our AUD sample. Second, consistent with the notion that impulsivity can be modified by contextual factors [25], individuals who participated in AA longer tended to show larger decreases in impulsivity across all assessment intervals.
References
Blonigen, D. M., Timko, C., & Moos, R. H. (2013). Alcoholics anonymous and reduced impulsivity: a novel mechanism of change. Substance abuse, 34(1), 4-12.