This is part of a series called “The Bottled Scream” A Disease of Self – Understanding Addiction and Recovery. To go back to the introduction click here.
Trauma
My mother’s dependency on Valium didn’t help much. As I explained eralier, she had been prescribed Valium soon after I was born (possibly before) and was dependent on it all her life. This meant that she mothered me in an emotionally distant, inconsistent and, frequenty, dismissive manner. She spent much of my childhood in her bedroom, bluntly asking me to leave her alone. Leaving me with the feeling it was my fault this had happened to her. A fear embedded into my heart that she never assuaged, a fear without a solution. She never recognised or addressed my fears and they were left to grow, my anger to simmer and boil over into rage.
I believe this lack of attachment and also in earlier in the first weeks and months, after being born, contributed to later introceptive and emotion processing problems. But much of the damage to my later life was done in infancy (and childhood) I believe. A damage, I think, coontributed to later addiction and C-PTSD. As we grow from infancy, our close bonds to our primary care giver is crucial for future development of our brains and our abilty to regulate our emotions, stress and ultimately ourselves (self regulation). In the first few months of life, the emotion and social parts of the brain that regulate emotion and distress develop during this initial two way relationship between primary care giver, mother in this case, and baby, me, which models behaviour that successfully regulate emotions. The brain architecture for emotion (and stress) regulation did not get properly manufactured in my brain. It did not mature properly and this led to later emotional immaturity.
I feel I was born into trauma, an attachment trauma, that I never fully bonded with my mother, the primary caregiver and ended up with a insecure attachment, one they call disorganised attachment, an attachment that provokes a fear without solution. In other to understand this type of attachment disorder, we can imagine a mother and son playing in a room, the mother leaves and a stranger comes into the room. When the mother returns and the child is reunited with the mother, following this period of absence, a child with disorganised attachment would experience inconsistent fearful reactions that never resolve themselves, such as approaching the mother initially, then stopping or falling to the floor, it is also called fear without solution. The child does not treat the mother as a secure attachment he can return or not, safe in the knowledge she is there when he needs her. He can return when he likes, he can explore, play or come back to her when he likes as she is there, cosistently available to his emotional needs.
The disorganised child is not sure that his mother, primary caregiver, is there in a consistent manner to care for him and his emotional needs, she is there sometimes, not always, she is inconsistent in her caregiving and he is insecure in his attachment to and bonding with her. His fear is not satisfactorily solved by his mothers caregiving. Her care and love seem conditional, based on her availabilty not on his emotional needs. This lays down a template in his mind about people and how available they are to him, it infuences his future reactions, an internal working model, that care and love are not always available or that they are available sometimes and not others. It leads to a fear of rejection.
A fear of not being deserving enough of unconditional love and care. It is a pattern of responding that can lead into later adolescence and adulthood. It can lead to a wide range of mental health issues, including C-PTSD and addiction, where “substances” become a type of “secure” attachment.
Unresolved fear.
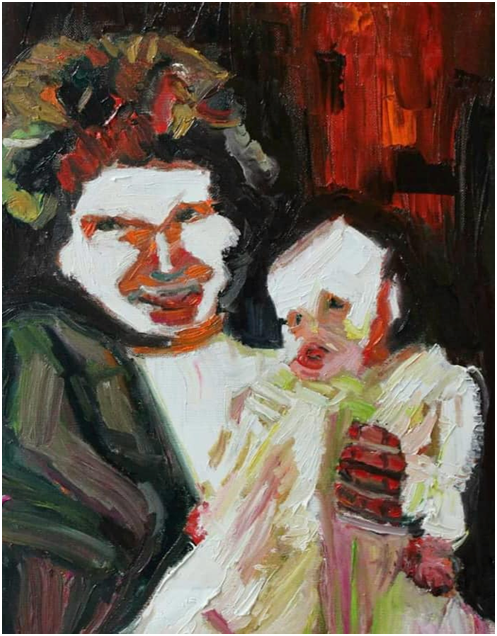
Even in later in life I would phone her armed with a tin of beer and a spliff. She unsettled me at a profoundly deep level. I was never sure of her, or safe in her presence, I was always guarded against rejection. I never felt fully secure although I loved her dearly. I was also inconsistent in my behaviour to her, especially in later life when I would exact petty revenges on her which sometimes involved abandoning her to see how she liked it. I remember once leaving her for hours with a portrait painter, a complete stranger, who made he feel very uncomfortable and anxious with his awkward questions as he painted her. Abandonment was what I felt in relation to her, even when talking to her on a phone call.
I felt I received conditional love from her although I believe and feel she loved me. It was through an emotional haze, she wasn’t fully present. She wasn’t fully available. I waited for a love that I would never fully receive. I waited for her to come for me but she didn’t and I grew up feeling strangly rejected and abandoned.
I internalised this as being my fault most of the time, sometimes unconsciously, as this “not being worth it” and this became part of my view of myself in relation to the world. My negative self perception automatically retrieved rom my negative self schema. I wasn’t worth it, I was defective in some way, not worth the effort. I wasn’t worth saving! So what did I do with my distress and my everdyay negative emotions. I buried them, suppressed them , didn’t share them. Sharing how you felt increased the chance of having them rejected. It was too painful to have then ignored and dismissed so I started blunting my emotion resposnes. Sometimes I would demand to be heard and overreact and my mother would shout to my father to have me taken away from her, to stop bothering her.
Eventually I realised my mother heard what she wanted to hear and that was rarely the truth so I tried to not having emotions as they were too painful, when not shared or reciprocated.
This led to a toxic shame and a blunted awareness of my feelings. It was as if shame was prompted by having emotional needs that were thwarted. Shame then became the overriding feeling and took control of my life. My emotions almost became servents to this overriding shame, it was the master emotion provoking self pity, guilt, selfishness, self centredness, arrogance, intolerance, impatience, anger, rage, greed, gluttony, and in later years, lust. The very same emotions I list on my Step 10 inventory every nght. The shame based respsonding I have to life today and have had since eary childhood. Traumatic and toxic shame, the beating heart of all addictive behaviour.
Shame contributed to my alexithymia, the inability to recognize or describe my emotions too, the numbing of emotional repsonse. The fleeing from feelings. My feelings were troublesome and best not having. It was best to ignore them and take your mind off them instead, to live outside them. To act outside of yourself without realising, the internal shame was constantly animating your every action. I was fixing my feelings from an early age. I could run away from them but I couldn’t escape them. They would catch up with me one day.
I now know it wasn’t her fault. She was suffering from addiction but I never knew that fully at the time. We were all suffering from addiction as a family, but this realisation came decades later. For me anyway. It didn’t come for mummy, we never fully discussed it. She was dead by the time I came into recovery. So in the absence of an acknowlegement of the terrible effects of addiction I instead waited, in my own undiagnosed addiction and alcoholism, for some recognition of a shared but troubled past she couldn’t, or wouldn’t, recall and re-examine as it may have been too emotionally overwhelming or she couldn’t reconnect with as she was fully involved in it initially.
I am trying to square that troubled past now in writing this book, to exorcise the ghosts of the past. To liberate us from our past. Memory recall often depends on the clarity and intensity of emotion that accompanied the episode remembered. Blocked off emotions weren’t conducive to this recall. For mummy it was if the past almost happned to someone else. It didn’t really happen to her because she wasn’t fully present at the time.
When I asked about the past it brought out angry reactions in her. She castigated me for dragging up the past so I cannot say if she had painful memories or didn’t want to contemplate her son’s pained reaction to the past. Emotions seemed to threaten to overwhelm her, before a shrug of the shoulders seemed to send them off, floating away on a distant cloud. As if they weren’t her resonsiblity, didn’t belong to her. She didn’t seem to care sometimes. It was as if she was about to have some emotional response then it would dissipate like passing clouds, the Valium wafting it away.
She made me feel sad, not deserving of anything more. Thre was no explanation or commiseration, no acceptance of even acknowledgement of my pain, no empathy. I never felt fully seen, fully felt in her unconditional love. There was no safe haven or resting place in her affection. There was no solution to my fear and emotional distress.
This made me feel strangely not worth the effort or time, somehow defective. She made me angry, raging even, especially in childhood. I dismayed she wasn’t like my friends’ mother. How come my mother was so odd, so detached? Or depressed and uncaring? So useless. Why didn’t she care about us enough to love us. Why did she have us in the first place if she didn’t want us? We were all a big mistake to her it seemed. Worthless. I sought attachment everywhere I could, of course. From my sisters, from my aunts. Friends and later from girlfriends. Anywhere I could find a fleeting solace and a place to rest from my errant painful emotions, for a while at least.
But is was precarious, I constantly guarded against a rejection I somehow was sure would come. It always did eventually, I felt. Later in life I would finish relationship with girls and woman before they did, just in case. The only constant relationship I had, that never rejected me was with alcohol, that was it until it sent me mad and almost killed me. I am so lucky that alcohol spat me out too otherwise I would have died.
It was a chemical attachment, a fairly consistent safe harbour. A solution to the fear and self loathing. A very, and increasingly crude solution. A medication just like my mother’s Valium. Strange how I never took Valium in case I became addicted like my mother? All the while slipping into alcoholism.
Decades of unresolved fear and emotion knawing away at my psyche, propelling me further and further into addiction and distress. I thought I was runnng away from my problems instead of running more deeply into them. Past addiction and trauma, the fuel for my present alcoholism. The alcohol, over years of chronic drinking, increasing the fear without solution. The fear becoming psychosis. My sisters suffered from this insecure parenting too and all the family dysfunction as a result of my mother’s Valium dependency. We all came second. Although my sisters probably didn’t always see it that way.
They thought, in my mother’s conditional love, I came first as the youngest child and only boy. God knows how little they received in terms of maternal love, if they were jealous of the scraps I got? I probably got more conditional love than they did, if that makes sense? They didn’t seem to have the same insecure attachment as me and grew up with ambivalent or anxious attachments rather than my disorganised attachment.
I believe we all grew up in the trauma of neglect and emotional abuse but I am not sure they ended up with C-PTSD and it’s associated dissocative disorder. Perhaps my initial attachment trauma left me more vulnerable to being traumatised by later traumatic events, some of which they witnessed too? Perhaps it affected me more as I was the youngest? Perhaps because I had already suffered from trauma, attachment trauma? It is difficult to say. Mental health problems, like alcoholism, are often self diagnosed, often with the help of competent professionals or through recovery circles. Most trauma, in life, seems buried in denial. I didn’t self diagnose my chronic alcoholism until it practically killed me or my C-PTSD until ten years into recovery when it threatened me with relapse. I had thought many times and discussed with my wife on numerous occasions that I had trauma issues but only I accepted my C-PTSD when I started to profoundly dissociate, on one occasion all the way back to childhood. I even spoke in a child’s voice on one occasion, spluttering out
“When I make mistakes people die!”