Addiction
This is part of a series called “The Bottled Scream” A Disease of Self – Understanding Addiction, Trauma and Recovery. To go back to the introduction click here.
Chapter 11
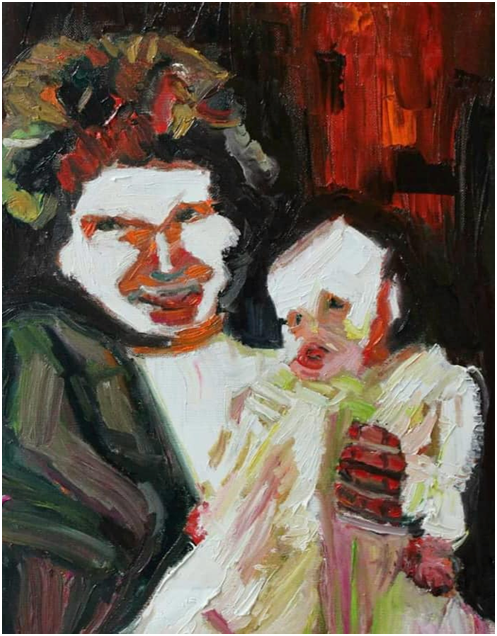
In early recovery, it is like you have two selves fighting it out.
I went to my first meeting a couple of days after becoming sober.
I went to my first meeting sober and it was hellish.
I spotted a couple of guys from the first meeting and they said hello. They were glad to see me which was nice. I tried to talk to them for a bit but felt too self conscious and scampered inside. I sat as far away from the Chair as possible.
I was still partly in psychosis, everyone was trying not to stare at me and my jaundice and the green discolouration snaking around my neck.
I sat beside the most fidgeting man who I was convinced was pulling faces scary faces and making menacing gestures towards me from out of the corner of my eye.
I couldn’t believe how slowly time was passing. Through my gauze-like eyes I was shocked how it always only 5 minutes later than the last time I looked.
It was tough being out in the world without the drink as a crutch.
It was like I was wearing my nervous sytem inside out.
I was so full of self pity, it threatened to drown me. Thoughts were like poisoned darts piercing my heart with terror, thousands of them, relentlessly.
It was the same format as before. I liked how they read out the solution, the 12 programme of recovery.
It was reassuring this programme had helped all these guys and might me as well. Although it was difficult to see how it would. It did mention being restored to sanity which gave me some hope. Although it said we came to believe we could be restored to sanity and I was some way off that.
I tried to listen to proceedings. It was a bigger meeting than the previous one.
Some people addressed me when they started sharing, saying “welcome to the newcomer” whereby everyone smiled weakly at the jaundiced guy. The most alcoholic guy they had ever seen.
I started to wish they would stop doing it, okay I’m here no need to keep going on about it.
Ther were so many times when I just wanted to get up and get out of there but to where?
There was literally no where to go. To the treatment centre were they paraded me around like a jaundiced freak?
Back to drinking?
The attic?
Where?
Nowhere is where. There was nowhere but here.
I tried to listen but stuggled to at times.
The voice of lies was constantly chirping away in my head. It was saying I didn’t need to be here, with these losers. Stay off the drink for a bit, sure, until the liver got back into shape. Give the booze a rest. Hit those pills for a day or two.
That alcoholism, does it even exist? Do these people know what they are talking about? The book they read from was from the 1930 s and since then nothing?
It is a cult.
Why didn’t the doctor recommend them, nobody did? None of the medical professionals.
Is this the best they can do. Really?
Maybe it wasn’t so bad.
That last lie took some digesting. I noticed my lying voice had no shame whatsoever.
If you let it rant for a while it would often shoot itself in the foot by saying something ludicrous.
Also when I asked it did it want me to drink, it would go quiet?
It never really said wouldn’t you like a nice cool drink, it was more sneaky?
I had been spiked with ecstasy eleven months earlier so maybe that was the reason why I ended up in psychosis, it suggested?
Similar maybe to the way I ended up in psychosis due to too much cocaine. Maybe I was just subsceptible to it?
Maybe it wasn’t the drink at all. Maybe I was tipped into it via being spiked? It had changed something in my chemistry, my nervous system. I wasn’t this mad before the spiking, the last time I gave up drinking?
Just go back to that, get daily exercise, that sort of thing.
But this, what is it? Religious do gooders. Better going to the Pioneers. This lot seem Protestant!?
And middle class?
Is this the right place for you?
Maybe it was the cummulative effect of too many drugs, maybe it wasn’t the drink at all? Lots of people drunk more than you? For much longer.
And these peope in AA talking about being out of control drunks, you weren’t really, like you rarely were fall down drunk, only on special occasions when friends dropped by unexpectedly, you were never arrested or ended up in hospitals. You are not even like these people?
These guys are amateur drinkers they just couldn’t hold their liquor?
And this spiritual malady, that’s just sinning and that solution is just confession and repentance.
Sin doesn’t drive you insane. Spiking does, not knowing the effect it had on your brain?
And on and on.
Look for the similarities they said, but where are they?
Thee are sinners who couldn’t hold their drink.
These are do gooders. Religous zealots.
All these thoughts rumbled on in this first meeting.
Why?
If I wasn’t alcoholic then why was I juandiced from alcohol addiction
I knew one thing for sure, I had become addicted. SO even if I wasn’t alcoholic, whatever that was, I had become addicted. I was an addict at least?
I had also once tried a spiritual solution to my problems years ago, so I did have problems going way back. Over many years, mental health problems. But that solution, the Buddhism, led to psychosis too?
Or did it just unearth it? Was it really there waiting to erupt to the surface?
Maybe that is what I have and drunk to calm it down but couldn’t in the end?
That isn’t a sin disease like this?
This arguing went round and round on in my head relentlessly.
The other way to explain it was that my alcoholism was using my own voice to talk to me. That it wasn’t me but my addiction using my inner voice?
This thought nearly made be ill, I put this insight down to my lingering psychosis…
I stopped briefly to learn my calming heart was still with me, strangely smiling at me, unconcerned about the madness in my head.
The thought came to me, non alcoholics don’t have a constant chirping in their heads about being alcholic or not. I would ask Emma this question later.
Then as if by co-incidence one guy shared about his head telling him lies all the time and he had been in recovery some time. Years.
My attention was pricked. He said that on a very good day his illness talks and he doesn’t Iisten and on a good day the illness talks and he listens and on a very bad day he listens and then talks back until his brain gets completely mangled and he doesn’t know one thing from another!
A few men and women laughed out loud or nodded their heads at this point in recognition.
They related to what he was saying so might have had the same problem too?
This guy was talking of something more than a sin disease, to my mind anyway, however reliable that was!?
He was talking about a mental health problem which was similar to mine. This mental health problem, this thinking disorder, made me drink, and drink and…
I listened for my illness to retort and it was quiet. For the first time I acknowledged a possibility that honest answers seemed to be an antidote to this lying voice. This would prove to be the case in Treatment also in the weeks and months to come.
If possible I would try to ignore it all together.
So for the first time this pithy adage gave me my first insight into this illness. It was my first experience of “hearing what you needed to hear” in an AA meeting.
It was a great way of putting it. I felt this guy was like me and me, him. I had real identification with another AA.
What he said didn’t come from the Big Book, however, it came from Treatment. Where there new things to learn there? Did they look at things differently ?
It was more an experiential wisdom, the cumulative knowledge gained from recovery, from the rooms of AA over the seventy years since the BB was written. It was from the lived in experience of AA members rather than from a book that seemed to be, in part, “frozen in time”.
I found this intriguing. It spoke my language.
I shared that I was glad to be there and was glad to get some response.
After the meeting people were friendly to me and all had an inner glow about them. They all told me to keep coming back.
It left nice to hear, to be asked to come back as if they wanted me too.
I had so little self esteem and l felt so worthless that any human kindness was welcomed. I felt like a freak, a monstrosity.
Any human kindenss melted that image a little.
I was so glad to see Emma when she arrived to take me home in what seemed like days later.
I would wait a few days before going back to AA
Maybe when I was less jaundiced and less crazy. ,
In my next meeting I called out during someone’s share “what do you mean by a spiritual awakening?” and was told he would tell me after the meeting. So much for less crazy?
He didn’t.
Probably took one look at me and thought it wasn’t worth the effort. I’d be gone soon enough.
I was none the wiser about this spirtual malady that was at heart of all my troubles and somehow made me this mentally ill.
People looked at me half in sympathy, half in pity, another half incongruity. How the hell do you get to be that alcoholic? Was it a World record?
I was the Steppenwolf of the AA meeting.
I have never seen any one in the rooms who looked as bad as me since?
I have never heard of anyome have alcoholic pyschosis for more than a few weeks and that was a tiny tiny percentage of alcoholics, less than .05%
They usually die before then.
At least, the early AA founders were like me. Maybe I wouldn’t have looked out of place then?
I asked someone to sponsor me, a guy I thought I could push around but who I later learnt had been inside twice for two separate attempted murders!
He didn’t look or act like a potential killer now, so he must be doing something right.
He must have had some sort of psychic change to go from that to the cuddly office worker he looked now!
He asked me how I got to meetings and I said Emma drove me.
He said get a bus to meetings from now on.
Maybe he wasn’t the right choice?
I did too, for the next meeting where I met a guy called Tony who offered to drive me there in future.
Although 5 days sober, the illness, the alcoholism, vocally active in my mind, somehow remained. It had somehow been embedded in my brain and still talked to me.
I was still troubled by these thoughts and more so, by the fact they wouldn’t go away. I had stopped drinking so why hadn’t my mind quietened down around thoughts of drinking?
Why was it still chirping way, day in day out? Although not always about drinking. Sometimes it just put me down, character assassinated me.
When I had stopped smoking, after twenty years of smoking, I didn’t have this incessant inner dialogue.
Or when I ceased my twenty year and daily cannibus use.
Why was the internal dialogue was incessant?
Life was too difficult without such questions to torture me. The illness centres in the mind as the Big Book says. Could we trust our own thoughts even. There was a lot more to this alcoholism, addiction than met the eye.
Anyway, I had my other voice, the one that was even harder to believe in, coming like a warm smile across my troubled heart with warm tidings that all will be well.
Day by day this voice coaxed me out into the world and guided my through it, however gingerly.
The doctor had said I needed to be outside in the sun light to reduce the jaundice. I went for more blood tests at the local hospital Pathology lab and people stopped to point at me and laugh.
It was fairly humiliating but fortunately I have experienced worse so put it into my “it’s all relative” filing system in my mind.
What if I’d had liver cancer!?
Ignorant people are never in short supply.
It struck me that much of early recovery was about memory and different memory systems in the brain.
My addiction would arise at times implicity from habit memory and almost compell me to do certain things, sometimes it would use explicit memories to provide an imagenery scene about drinking and sometimes my brain would just freeze and I couldn’t shake it off. It was a locked in attention to drinking that happened again without my volition.
Was there anyway I could change these realities? The only way was to change my memories somehow?
To look back at these memories and reappraise them. I had started doing this already with my sponsor. He told be Step one work in Treatment would be looking at this for a few months.
We would discuss something and reappraise the past to show how it was really. It illustrated my memories were unreliable and gave false readouts on the past.
My memory couldn’t be relied on either it seemed. My thoughts and emotions and memories and sometimes even my perception of things all seemed a bit faulty.
He assured me the memory problem would be fixed via the steps 1 then 4 and 5 especially. Other problems could be ironed via sponsorship. I was to ring him whenever I needed to. It was surprising how often this was as I kept getting the wrong end of the stick over so many things in life. I didn’t seem to have a clue about living life on life’s terms. It was as if I would have to learn again from stratch. I could see why they call newcomers “babies” in US AA.
Another route, via memory, by which this illness trapped me was via my very negative self schema, which is a collection of memories and conditoning from the past which added to a condensed summary of how we feel about ourselves.
My self schema was very poor, full of shame and self loathing.
My illness fed on this, saying I wasn’t worthy of recovery.
This would have to be worked on too.
A possible clue to a solution was via an AA’s share, at this meeting, when he said his shame at being an alcoholic was relieved day by day by being proud of being an alcoholic in recovery, gradually through time, his shame lessened and his pride of being in recovery increased. His sense of self and his self schema and his esteem increased. He became more worth it. His self schema gradually changed and the illness had less to feed on.
It was a message of hope to think that changing how we felt about ourselves would help with recovery, that our twisted view of our past could be ironed out and that the habitual nature of addictive behaviour could be met with the habitual nature of recovery.
He was down the line from me, a beacon of how I could become, of how recovery could work for me too .
If I could only stay in recovery?
None of this was explicitly stated it the BB but it is there implicity in AA recovery and by product of it, if nothing else.
I would start working on my memories, they are what make us how we are, starting with my self schema with myself as an alcholic in recovery.