Most of my distress and emotional pain in recovery comes from wanting stuff, and not getting my way or not accepting things as they are.
As Bill Wilson noted, we seem to get distressed when we don’t get what we want or feel people or trying to take away what we have.
This was his observation after a decade of psycho analysis with the psycho analyst Harry Tiebout.
A decade of therapy also showed Bill Wilson he has two default settings in his relationship to other human beings – he either tried to dominate them or he became dependent on them for his sense of self and emotional well being. In other words, he became dependent on others, on external means for approval and elevating his self esteem.
This is similar to relying on external means, i.e. alcohol, drugs, addictive behaviours to regulate our emotions and bolster our low self esteem.
We are in a sense co-dependent on other people for our sense of esteem. We rely on others in terms of how we feel about ourselves.
As a result we are guarded against those that we perceive will reject us or be negative to us, harm us in some way and we seek to dominate these folk or we are dependent on those who are kind to us, help us and care for us. We swing at times between these extremes.
Some of us are “people pleasers”, some of us are dismissive towards others. I can be a dismissive person more than a people pleaser. It is all manipulating our interaction with others to our selfish ends.
Some of these tendencies are the result of our childhoods and how closely attached we were to our parents.
Some of us have this knawing feeling of not being good enough, have a hole in the soul which we are/were kinda always unconsciously trying to protect, shield from the world.
It is a strange feeling of not wanting to be found out of being less than, not good enough. “If people realise what the real me is like, they will reject me!” type thinking although a lot of this is unconscious and does not pop in to our minds as thoughts but is an unconscious self schema that shapes our behaviours.
In simple terms we manipulate via people pleasing or we push people away via being dismissive and putting others down, we guard against any threat of perceived rejection or threats to the self via defense mechanisms such as projecting what we do not like about ourselves on to others.
We often do not like traits in others because they somehow mirror traits in ourselves although we are not always conscious of this.
We have difficulties in our relationships with others, these relationships are often unhealthy and ill.
Some of this is touched on in the Big Book of Alcoholics Anonymous, but much of it comes from later observations by Bill Wilson after the publication of the Big Book and my and others’ observations since.
I have seen in myself how fear and shame seem to drive most of my maladaptive behaviour.
My illness of addictive behaviours.
I have an illness of chronic malcontent, things are rarely good enough and I am rarely good enough, according to my “out of kilter” thinking which I usually try to ignore, turn over to God or on occasion challenge via reasoning and sharing with other people.
My thoughts are often not my friends, they are often not in the service of my ongoing well being, quite the opposite in fact.
This is how a mental health disorder manifests itself as distorted fear based thinking which appear, if acted upon, to make one’s situation a whole lot worse.
We can not rely on our thoughts and feelings or, in other words, our Self Will. Our self will has become impaired and is no longer in the service of our successful survival.
I have found over the last decade in recovery that when I turn my Will over to the care of the God of my understanding that I am restored to sanity and my thoughts are sound, they are on a higher plane as the Big Book tells me.
I can become the fullest expression of me in the God, not the ill, deluded version while running under my own self will. That has been my experience.
It is only with God’s help that I get restored to sanity or reasonableness.
When I have a fear of not getting stuff and this is linked to insecurity, as mentioned in the Big Book, it is usually in relation to my pocket book, financial insecurity, personal relationships, self esteem etc.
I will now look at this fear based reaction to my security which is mainly to do with stuff out there (external) such as work, people and how they affect my sense of self before looking at how my internal sense of self, based on the fear based emotion of shame seems to play a pivotal role in my relationship with others and the world around me.
I am assailed externally by fear of what other’s think about me and internally about what I think of me – when these two line up it can have a powerful and damaging effect on my psyche.
Desiring stuff seems at the root of my fear based stuff – the exquisite torture of desire which soon loses it’s so-called relish and just becomes torturous.
Alcoholics do not seem want stuff like normal folk, but have a pathological wanting, an all consuming need to get stuff regardless of it’s worth or value.
We seem to compulsively seek to relieve an inherent distress of not having what we set out to get. Our decision making seems fueled at times by this need to relieve distress rather than the intrinsic value of what we are seeking.
We seem to become manic in our pursuit of things and end up overdoing whatever we are doing via this stress-based manic activity.
This seems compounded by not always being able to read our emotions or somatic states.
One of my own difficulties is realising I am hungry or tired and I can often end up exhausted by over-doing stuff especially manual work around my house. My stop button broke a long time a ago and probably did not work very well to begin with.
So we have stress-based compulsive need to do something and very limited brakes in the brain stopping us and very little emotional feedback going on, a limited consideration of “aren’t we overdoing this a bit?”
Desire obviously runs contrary to the idea of being in God’s will, in fact it is being in Self Will that seems to create distress in many people with addictive behaviours.
I would add to this that I also get distress via fears of rejection from others, I suffer from fear based shame to a chronic extent.
Shame, also the consequence of being in Self Will, was not really mentioned in the Big Book of Alcoholics Anonymous, mainly because it was not really known about as a psychological or psycho-therapeutic concept then.
Much of the Big Book was influenced by psycho-analysis which did not consider shame, but rather guilt, in psychological disturbance.
In fact, it has only started considering the role of shame in the last few decades.
So I would add fear of not getting what we want or having something taken away is also complemented by shame-based fears of being rejected.
For example there is an undercurrent in fear of things being taken away, of it being because we are not good enough, deserving enough, have failed in some way, which are shame based reactions.
In fact the Big Book gives me a good idea of the “sins” or “defects of character” I have when I have a resentment but does not explain why I have resentments in the first place.
It explains this as selfishness, self centredness… the root of all our troubles.
It does not, for me, clearly explain why we resort to these selfish, immature, emotional reactions or why we persist with resentments?
It does not explain the emotional immaturity at the heart of alcoholism, this spiritual malady of inappropriate emotional response to the world around us?
Bill Wilson was struck himself, when he started working with other alcoholics, how much they were plagued constantly by various resentments. How they were haunted by memories of situations in the past, how they swirl around and pollute their minds in the present. How they could not let go of events in their past?
For me he was seeing the root of this spiritual malady, this emotional disease.
For me we engage futilely and distressingly in resentment because we have an inability to process and control our emotions, they overwhelm us and we often react by people pleasing (shame) or react via various defense mechanisms (also shame based).
Defense mechanisms are central to psycho-analytic thought – such as projection etc, the idea that we expel “out of ourselves what we do not like about ourselves onto others.
Sometimes others expel the same negative emotions on to us. I have found this a fairly common trait among male alcoholics in recovery settings and meetings.
I was discussing this with a newcomer last week, how people who seek to “put us down” do so out of shame and induce in us all the negative emotions they are experiencing themselves!
The newcomer gave me an example of a resentment he was experiencing after this guy at a meeting said “get off your pink cloud” a phrase that refers to the sometimes mildly ecstatic feelings of early recovery.
This made the newcomer ashamed that he could have been so stupid for being on this pink cloud, as if this was a selfish indulgence!?
I explained to him that his pride had been hurt, he was in shame and his “apparent” depression every since was simply prolonged self pity.
If we leave self pity to fester long enough it becomes depression, that is my experience anyway.
I said the other guy was probably “hurt” to see a newcomer having such a good period of recovery (God does want us to be happy, joyous and free after all) – I said his false pride was hurt too, that he was not having the recovery experience at present of the newcomer (possibly because he wasn’t putting the effort in) and was in shame (not good enough) and self pity. This mesh of negative emotions can link up fairly instantaneously I find. It is the web my spiritual malady seeks to ensnare me in.
The guy was probably in guilt too as he could been working on his recovery more.
As a result this guy put the newcomer down to alleviate his own sense of self, his low self esteem.
He “had to” react with arrogance, dismissiveness, impatience and intolerance, because his shame, which is a fear based emotion, made him fearful of his own recovery and fear makes one strangely dishonest (at times deluded), This is my experience.
All because a newcomer had the temerity to be enjoying his recovery?
Not completely, this is half the answer.
The other part is that this guy, if an alcoholic like me, has real difficulties accessing in his heart and mind how he actually “feels” at any particular time. Or rather what emotions he is experiencing at any particular time.
This guy could have been experiencing guilt or shame for example.
Instead of saying to himself I am feeling guilt that my recovery is flabby compared to this newcomer or that I am being an arrogant “know it all”, putting this newcomer in his place because he had been in recovery longer – although being in recovery and being sober are different things I have found.
Either way, if he could perhaps of had the ability to say this is how exactly I am feeling he could have acted on this emotional information rather than reacted to it.
What do I mean by this?
Well, if I was feeling guilty about this newcomer it would cause a disturbance in me because I have difficulties processing my emotions.
It would have turned up therefore as a resentment of someone having something I do not have and as them taking away the illusion that my recovery was going OK?
I would have found this threatening to my sense of self so I would have reacted via defense mechanisms. I would have strangely blamed this person for making me feel the way I did! Even if this person had no such intention of hurting my feelings I would blame him nonetheless via my defensive reactions.
It is as if my emotional well being is dependent on other people and their behaviours, this is my spiritual malady, my emotional disease.
As I would have had a resentment, it would have had a wolf pack of negative emotions attached.
In this instance I might have have acted differently.
If I had been in God I would have been more sane for a start and had more loving tolerance for a newcomer.
I would have been acting not reacting. I would have had empathy for where the newcomer “was at in his recovery” as I had been there once too.
This love and tolerance for the newcomer evolves the displaying of virtues (the opposite of defects are virtues).
What virtues? Well as the newcomer was relatively new I would attempted to be patient, empathetic, kind, gentle, tolerant, considerate etc. These prevent the defects occurring I find.
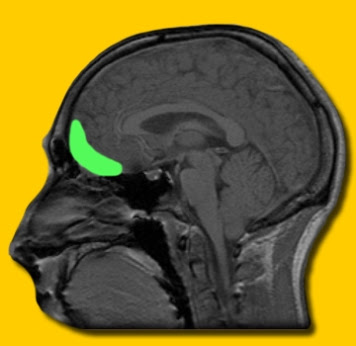
If we practice virtues instead of defects then the brain changes for the better and we recover quicker. Our positive loving, healthy behaviours change us and our brains via neuroplasticity for the better.
Attempting to live according to God’s Will (which is a state of Love) also helps me not react but to act with Grace.
In Grace we can still experience negative emotions but God allows us to see them for what they are and not react. His Grace takes the distress out of thee negative emotions. This is my experience.
This allows me to do a quick inventory of my negative emotions and a prayer to God to have them removed. My experience is that they are always removed and that we are immediately restored to sanity.
I do not necessarily have to react to my feelings of negativity about myself, someone else does not need to experience the consequence of my resentments.
I can manage my spiritual malady or emotional dysfunction, I have the tools to do so.
I also impressed upon the newcomer that what the other guy was experiencing and was reacting is also how he, the newcomer, reacts and how I react too.
It is what our spiritual malady looks like I believe, it is the map of my impaired emotional responding.
I also impressed upon him that mostly I can manage this emotional dysfunction but often I fail to and get into a resentful anger.
This is why I have to forgive the other guy as I have been forgiven but also to forgive myself (or ask God to forgive me my shortcomings) for my reactions.
We are not perfect, far from it. We are far from being Saints but have a solution Saints would approve and achieve a kind of transient sanctity in this 12 step solution of letting go and letting God.
We have to show love and tolerance for each other as we suffer the same illness/malady. Dismissing others like us for having what we have and acting as we do is like a form of self loathing. We have to forgive ourselves and each other for being ill. Self compassion allows us to be compassionate towards others.
Also we need to be aware what we project on to other alcoholics is the same thing as they project on to use and sometimes we project if back.
So we have two main ailments, distressed based wanting which results in the same negative emotions as being in a shame- based fear of rejection.
I can get out of the distress of wanting/needing stuff by asking God to remove those negative emotions which block me off from Him.
For example, if I really want something and feel someone is preventing me getting that thing or that they are taking this thing away from me I have a hunting pack of negative emotions running through by heart and pulsating through my veins, propelling me to want that thing even more! As if my very life depended on it?
These feelings are translated as “how dare you take that thing/stop me getting that thing” – False Pride – followed by fear of being rejected – Shame (this is because I am not good enough) and possible Guilt (for something I must have done wrong as usual) – then leading to “poor me” and feelings of Self pity, all because I am in Self, so I am being Self Centred and not considering someone else’s view so I am Selfish.
I retaliate via by “I”ll show you/I’ll get you” emotions of Dismissiveness, Intolerance, Arrogance and Impatience – my “I’ll put you down to make me feel better!”
All because I am fearful that you are taking away something from me or rejecting me – Fear and Fear is always accompanied by dishonesty.
I will act out on these somethings, if I do now use my spiritual tools and let Go and Let God, usually by eating too much, Gluttony, having a shopping spree, Greed, engaging sexual fantasy/activity Lust of “freezing” through fear in the subltle sin of Sloth (procrastination).
A perceived slight or a rejection can have an incredible emotional effect on me
This is all emotion dysfunction and immaturity. I have resentments because they are a true sign of emotion dysfunction.
The mature way to to access, identfiy and label how one is feeling and use this information to reasonably express how one is feeling. This way we do not retaliate, fight, flee or freeze. Instead our emotions do what they are supposed to do. They are suppose the tell the fronts of our brains to find words for our feelings. Not to tell the bottom of our brains to fight back or run or freeze.
Let me use an example.
I had an argument with a guy once who suddenly proclaimed he was upset by what I had said. I was amazed as this guy was reading his emotions, identifying verbalising/expressing them to me in a way I have never been able to do.
My alcoholism is rooted in an impaired ability to read, identify, label and express my emotions (otherwise called emotion processing) – as a result my emotions have always troubled me and been so troubling in their undifferentiated state that I have always either avoided them or ran away from them.
I have sought refuge from my negative emotions in alcohol, drugs and other addictive behaviours. It is this that propelled my addictions, this inability to deal with my negative emotions. I dealt with them externally via addictive behaviours, not internally via emotion processing.
My emotions became wedded in time to being undifferentiated arousal states that prompted me to seek an external way to deal with these troubling emotional/arousal states.
Today when I engage in the above emotion dysfunction, engage in the above web of defense mechanisms it is because I have not been able to locate in me what feeling is disturbing me ?
On occasion it is, as the guy above said, because I am upset. I have not learnt the ability to say that I am upset etc. The words for these feeling states somehow can continue to elude me unless I am in God’s Grace.
God does for us what we can not do for ourselves!
Finding out what is really going on with us emotionally is at the heart of recovery. That is why we have to constantly share how we are feeling with others so that we can find out what we are feeling.
Unless, we let Go and Let God and ask God to remove these negative emotions/sins/defects of character we end up in a futile increasingly distressed spiral of negative emotions.
We end up cultivating much greater misery.
As soon as you can, let Go and Let God.