In various blogs we have suggested that one of the main aspects of addictive behaviours is to act as the result of distress-based impulsivity or negative urgency. Here we explore in more details what we mean by that term negative urgency. Here we borrow from one article (1) which has an excellent review of negative urgency (1). The experience of emotion facilitates action. It has long been recognized that emotional processing appears to prepare the body for action (Frijda, 1986; Lang, 1993; Saami, Mumme, & Campos, 1998). In fact, to emote means, literally, to prepare for action (Maxwell & Davidson, 2007). Researchers have theorized that the relationship between emotional experiences and actions involve activation of the motor cortex by limbic structures (Morgenson, Jones, & Yim, 1980). Some investigations have used neuroimaging techniques to document increased activity in motor areas of the brain during emotional processing (Bremner et al., 1999; Rauch et al., 1996), and nonhuman studies suggest the emotion-action interface may involve connections between the amygdala and the anterior cingulate cortex (ACC: Devinsky, Morrel, & Vogt, 1995). Hajcak et al. (2007) found that emotionally arousing stimuli increase motor cortex excitability. The authors theorized that there may be individual difference in emotional reactivity that may relate to differences in the amount of activation of the motor cortex areas. One takes action to meet the need identified by the emotion.Pinker (1997) makes this point by noting that “Most artificial intelligence researchers believe that freely behaving robots . . . will have to be programmed with something like emotions merely for them to know at every moment what to do next” (p. 374). Intense emotions can undermine rational, advantageous decision making (Bechara, 2004, 2005;Dolan, 2007; Driesbach, 2006; Shiv et al., 2005). It also appears to be true that attempts to regulate negative emotions can impair one’s ability to continue self-control behaviors (Muraven & Baumeister, 2000; Tice & Bratslavsky, 2000; Tice,Bratslavsky, & Baumeister, 2001). Thus, it is not surprising that individuals engage in other strategies to manage intense emotions that are ill-considered and maladaptive, in that they work against one’s long-term interests. For example, heavy alcohol use may be used to manage emotion. Daily diary studies of alcohol use indicate that individuals drink more on days when they experience anxiety and stress (Swendson et al., 2000). Indeed, negative affect states have been shown to correlate with a greater frequency of many maladaptive, addictive behaviors, including alcohol and drug abuse (Colder & Chassin, 1997;Cooper, 1994; Cooper et al., 2000; Martin & Sher, 1994;Peveler & Fairburn, 1990). This pattern also is true of bulimic behaviors; individuals tend to participate in more binge eating and purging behaviors on days during which they experienced negative emotions (Agras & Telch, 1998; Smyth et al., 2007). Emotions such as shame, guilt, anger, depression, loneliness, stress, anxiety, boredom, and rejection are often cited as triggers for binge and purge episodes (Jeppson, Richards, Hardman, & Granley, 2003). For bulimic women, engaging in binge eating produces a decline in the earlier negative emotion (Smyth et al., 2007). Because actions like these do appear to reduce negative affect, they are reinforced. Brain Pathways Related to Emotion-Based Action Brain system involved in emotion and action -the amygdala, the orbitofrontal cortex (OFC) and its medial sector (the ventromedial prefrontal cortex, or VM PFC:Bechara, 2005), and other areas of the prefrontal cortex (PFC:Barbas, 2007). The amygdala appears to be heavily involved in the experience of negative affect; more broadly, it is thought to play a role in directing attention to emotionally salient stimuli, particularly stressful or disturbing stimuli (Davidson, 2003).
The OFC appears to be involved in the modulation of emotion-based reactivity (Davidson, 2003). OFC activity overrides emotional responses, apparently by providing information and a bias toward long-term, goal-directed behavior (Lewis & Todd, 2007). Davidson and his colleagues (Davidson, 1998, 2000,2003;Davidson & Irwin, 1999; Davidson, Putnam, & Larson, 2000) suggest the experience of intense emotion, and its accompanying potential actions, is inconsistent with one’s long-term goals. The OFC, perhaps particularly the left VM PFC, provides a biasing signal to avoid immediate reward, and thus maintain one’s pursuit of one’s longer-term goals. Davidson (2003) refers to this process as affect-guided planning and anticipation: with healthy left VMPFC functioning, one gains access to the emotion associated with anticipated outcomes consistent with one’s long-term goals. The ability to do so is, Davidson argues, the hallmark of adaptive, emotion-based decision making. At times, long-term affect-guided planning is difficult: the experience of intense emotions unrelated to one’s long-term interests may disrupt processing with regard to those interests (Gray, 1999; Preston, Buchanan, Stansfield, & Bechara, 2007). But healthy functioning of the left VM PFC helps one maintain an affective connection to one’s longer-term goals, and thus plan accordingly. Damage to the OFC, and perhaps damage specifically to the VM PFC, results in affective lability and rash action particularly in inhibiting the action of amygdaloid reactivity.
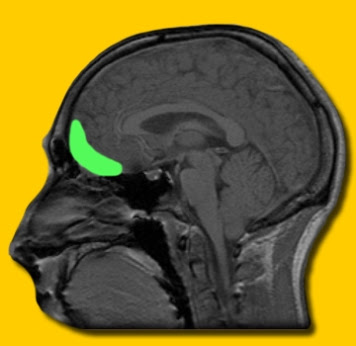
————————————————- The authors of this study put forward various reasons why OFC and VM PFC damage can cause rash action – we consider these before forwarding our own ideas of why OFC/ VM PFC damage may prompt distress based impulsivity. The OFC, perhaps particularly the left VM PFC, provides a biasing signal to avoid immediate reward, and thus maintain one’s pursuit of one’s longer-term goals. Davidson (2003) refers to this process as affect-guided planning and anticipation: with healthy left VM PFC functioning, one gains access to the emotion associated with anticipated outcomes consistent with one’s long-term goals. Activation of the left VM PFC also appears to inhibit amygdalar activity (Davidson, 1998), thus shortening the time course of the experience of negative affect and attention to stressful stimuli. Because negative affect stimulates autonomic nervous system (ANS) activity, which provides support for action in response to distress, prolonged negative affect leads to prolonged ANS arousal (Davidson, 2000). Perhaps a greater duration of ANS arousal increases the likelihood of affect-triggered action. Activity in the amygdala appears to facilitate this process. Damage to the OFC, and perhaps damage specifically to the VM PFC, results in affective lability and rash action. Individuals with PFC damage, and with OFC damage in particular, do not; they do not appear to have the normal anticipatory affective response to potential punishment (Bechara, 2004; Bechara, Tranel, Damasio, & Damasio, 1996; Cardinal et al., 2002). Thus, OFC damage appears to impair affective anticipation of potential risk to one’s actions. Bechara, Damasio, Damasio, and Anderson (1994) described OFC-damaged individuals as oblivious to the future consequences of their actions, but sensitive to immediate reinforcement and punishment. Thus, their actions tend to be guided by immediate consequences only. These patients had otherwise retained their intellectual capacities, including abstract reasoning skills. They could even describe possible future consequences in realistic language. They appeared simply to lack the anticipatory affect that others have; thus perhaps lacking the affect-guided anticipation described byDavidson (2003). The authors then suggest that associations between the OFC/VM PFC-amygdala system and psychopathy are consistent with their claim of an association between this system and the urgency traits. In other words, individuals high in psychopathy have reduced VM PFC functioning, and hence lack an affective connection to the consequences of their actions. Other studies have also documented similar OFC functioning deficits among psychopaths (Blair et al., 2006; Mitchell, Colledge, Leonard, & Blair, 2002). This model is interesting but there is not mention of stress systems in this model although the authors mention distress and negative affect but not the stress chemicals underpinning these affective manifestations. The authors also do no mention two hugely important points we believe; a. that this amgydaloid (hyper) activity, caused by PFC dysfunction can also “offline” PFC activity (fig.1) b. in favour of the compulsive, emotive-motoric behaviour of the dorsal striatum which drives rash action, distress-based impulsivity or compulsivity rendering the individual remote to negative consequence of actions, although he/she may be able to explain clearly these consequences. prior to or after seeming to not consider them. It is chronic stress dysregulation in addiction that “cuts off” access to action-outcome or goal-directed parts of the brain and recruits stimulus response, implicit, “must do” action instead. fig 1. This we believe is the mechanism of negative urgency rather than as the authors suggest in this article, but not included, that VMPFC damage renders individuals unknowing of consequence, when rather, consequence, negative or otherwise, has been cut off by this amygdaolid activity rendering action outcome associations remote to consciousness. The brain acts implicitly, procedurally or in a stimulus response way to distress we believe in addictive disorders when heightened amgydaloid reactivity is in charge of behaviour with VMPFC deficit contributing to this amgydaloid dysfunction. An argument against simply seeing rash behaviour as the result of OFC or VMPFC damage which leads to lack of knowledge of consequence is that it does not really consider the chronic stress that accompanies addictive behaviours and which creates a near constant distress which acts in the way we describe above. This does not mean that there is a lack of emotionally guided behaviour or action on the part of addicts. It would appear, as discussed in previous blogs, that emotional processing deficits are common in addiction and may not recruit the goal-directed parts of the brain as the authors suggest. They do not guided action or choices effectively. As a result they manifest in perhaps crude, undifferentiated or processed forms as distress signals instead and recruit more limbic, motoric regions of the brain. Hence they are not use to anticipate future, long term consequence. We are simply adding that as addiction becomes more chronic, so does stress and emotional distress and this appears to lead to a distress-based “fight or flight” responding to decision making that the authors have mentioned in this article but not elucidated as above. Addicts increasing appear to recruit sub-cortical or limbic areas in decision making and this is prevalent in abstinence as in active using. it is the consequence of chronic and stress dysregulation. We suggest that this chronic stress prompts negative urgency via an hypofunctioning ACC (2) and by a “emotional arousal habit bias” as seen in post traumatic stress disorder (3) whereby chronic emotional distress increasingly during the addiction cycle comes to implicitly activate dorsal striatal responding “offlining” the PFC in a similar manner to fig. 1. References 1. Cyders, M. A., & Smith, G. T. (2008). Emotion-based dispositions to rash action: positive and negative urgency. Psychological bulletin, 134(6), 807. 2. Li, C. S. R., & Sinha, R. (2008). Inhibitory control and emotional stress regulation: neuroimaging evidence for frontal–limbic dysfunction in psycho-stimulant addiction. Neuroscience & Biobehavioral Reviews,32(3), 581-597. 3. Goodman, J., Leong, K. C., & Packard, M. G. (2012). Emotional modulation of multiple memory systems: implications for the neurobiology of post-traumatic stress disorder.
|
anterior cingulate cortex
At Risk Adolescents have Emotional Dysregulation?
Following up from our previous blog on the abnormalities in the ventromedial prefrontal cortex (vmPFC) in alcoholics, brain regions which govern emotional regulation, we came across another study which appears to show that adolescents at increased risk for later alcohol use disorders (AUDs) may also be showing an emotion regulation difficulty.
This emotional regulation difficulty may be a biomarker for later alcoholism, which is in keeping with our previous proposals that an emotional processing and regulation difficulty or disorder underpins the aetiolgy of of alcoholism. In order words it is part of the pathomechanism – or the mechanism by which a pathological condition occurs- of later alcoholism.
The area in this study, the vmPFC, showed relatively increased cerebral blood flow (CBF) in bilateral amygdala and vmPFC and relatively decreased CBF in bilateral insula, right dorsal anterior cingulate cortex (ACC) and occipital lobe cuneus of high-risk adolescents. This suggests that adolescents at relatively high-risk for AUD exhibit altered patterns of resting CBF in distributed corticolimbic regions supporting emotional behaviors.
The authors’ hypothesized that the relatively increased amygdala and ventromedial prefrontal CBF may contribute to increased emotional reactivity and sensitivity to environmental stressors in these individuals while diminished insula/occipital cuneus and dorsal anterior cingulate cortex (ACC) CBF may lead to poor integration of visceral and sensory changes accompanying such emotional stress responses and top-down regulation of amygdala reactivity.
Thus we see our model in a snapshot even in adolescents potentially. The emotional processing deficits we have discussed previously implicate the insula and ACC, as there appears to be a difficulty in alcoholics in reading emotional or somatic signals/states and integrating these signals into the identifying, labelling and processing of emotions. Equally there appears to be a hyperactivty in the vmPFC and amgydala as with alcoholics which implies emotional dysregulation, a hyper reactive emotional response and a tendency perhaps to a more “fight or flight” response, distress based impulsivity and short termist decision making, wanting it NOW rather than later.
References Lin, A. L., Glahn, D. C., Hariri, A. R., & Williamson, D. E. (2008). Basal Perfusion in Adolescents at Risk for Alcohol Use Disorders. In Proc. Intl. Soc. Mag. Reson. Med (Vol. 16, p. 60).
Emotional Dysregulation, recovery and relapse
Throughout our blogs thus far, we have attempted to highlight how emotional dysregulation appears to prevalent to all aspects of alcoholism and addiction from pre-morbid vulnerability to endpoint compulsive addictive behaviours.
Here we highlight a few articles which have considered how prevalent is emotional dysregulation in alcoholism and addiction in early abstinence/recovery.
Early abstinence from chronic alcohol dependence is associated with increased emotional sensitivity to stress-related craving as well as changes in brain systems associated with stress and emotional processing.
Early abstinence from alcohol is associated with changes in neural stress and reward systems that can include atrophy in subcortical and frontomesal regions (1).
Moreover, recent imaging studies have shown that these brain regions are also associated with the experience and regulation of emotion (2).
While alcohol-related changes in emotion, stress and reward-related brain regions have been well documented difficulties in emotion regulation (ER) have not been studied much.
One study (3) examined ER in early abstinent alcohol-dependent individuals compared with social drinkers using the Difficulties in Emotion Regulation Scale (DERS).
The DERS is an inclusive scale and defines ER in terms of four major factors: the understanding of emotion, the acceptance of emotion, the ability to control impulsive behavior and the ability to access ER strategies benefiting the individual and the specific goals of the situation. The scale has been validated in cocaine dependent patients (4) and on alcohol dependent individuals.
ER difficulties in treatment-engaged alcohol dependent (AD) patients during a period of early abstinence that is marked by an overall distress state. AD patients reported an overall problem with emotion regulation compared with SDs in the first few days of abstinence; in particular with emotional awareness and impulse control. Following protracted abstinence, AD patients significantly improved awareness and clarity of their emotional experience, and only significant problems with impulse control persisted.
This is consistent with neuro-imaging studies showing chronic alcohol abuse to be associated with stress and cue-related neuroadaptations in the medial prefrontal and anterior cingulate regions of the brain (6), which are strongly implicated in the self-regulation of emotion and behavioral self-control (7). As impulsivity in distress states may reflect a change in priority from self-control to affect regulation (8 ).
As we have seen in other blogs and articles (5) these areas are those which improve in short term abstinence/recovery.
Cocaine-dependent individuals also report emotion regulation difficulties, particularly during early abstinence (4). Additionally, protracted distress-related impulse control problems suggest potential relapse vulnerability Difficulties concerning emotional clarity and awareness compared with controls were observed which suggests that cocaine dependent individuals were less able to acknowledge and/or have a clear understanding of their emotions.
Clarity and awareness of emotions could represent early processing components of emotional competence (9) and may be integral to the maintenance of drug use.
The cocaine addicts appeared to have greater difficulty in developing effective emotional coping strategies (i.e. they would be more likely to believe that little could be done to change an emotionally stressful situations.) They were also found to report significantly higher scores on the Impulse subscale of the DERS compared with controls, indicating difficulties with regard to inhibiting inappropriate or impulse behaviors under stressful situations which can prompt relapse.
References
1. Bartsch, A. J., Homola, G., Biller, A., Smith, S. M., Weijers, H. G., Wiesbeck, G. A., et al. (2007). Manifestations of early brain recovery associated with abstinence from alcoholism. Brain, 130(Pt 1), 36−47
2. Fox, H. C., Hong, K. A., & Sinha, R. (2008). Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addictive Behaviors, 33(2), 388-394.
3. Ochsner, K.N., Gross, J.J., 2005. The cognitive control of emotion. Trends Cogn. Sci. 9, 242–249
4. Fox, H. C., Hong, K. A., & Sinha, R. (2008). Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addictive Behaviors, 33(2), 388-394.
5. Sinha, R., & Li, C. S. (2007). Imaging stress- and cue-induced drug and alcohol craving: Association with relapse and clinical implications. Drug and Alcohol Review, 26(1), 25−31.
6. Connolly, C. G., Foxe, J. J., Nierenberg, J., Shpaner, M., & Garavan, H. (2012). The neurobiology of cognitive control in successful cocaine abstinence. Drug and alcohol dependence, 121(1), 45-53.
7. Baumeister, R.F., Heatherton, T.F., Tice, D.M., 1994. Loosing Control: How and Why People Fail at Self-regulation. Academic Press, San Diego, CA
8. Tice, D.M., Bratslavsky, E., Baumeister, R.F., 2001. Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! J. Pers Soc. Psychol. 80, 53–67.
9. Salovey, P., Stroud, L.R., Woolery, A., Epel, E.S., 2002. Perceived emotional intelligence, stress reactivity, and symptom reports: further explorations using the trait Meta-mood scale. Psychol. Health 17, 611–627
How meditation helps with “emotional sobriety”!
In this blog we have considered two main and fundamental areas:-
1. that alcoholism appears to be an emotional regulation and processing disorder which implicates impaired functioning of brain regions and neural networks involved in regulation and processing emotion such as the insular cortex, anterior cingulate cortex and dorsolateral prefrontal cortex.
2. that in early and later recovery there appears to be increased functioning in these areas especially the dorsolateral prefrontal cortex (dlPFC) and anterior cingulate cortex (ACC) which is important not only in regulating emotions but also in abstinence success.
Our third point is that mediation, of various types, appears to strengthen the very areas implicated in emotional regulation and processing, which ultimately helps with “emotional sobriety” and long term recovery.
Various studies have shown that mindfulness mediation training in expert meditators, as well as novices, influenced areas of the brain involved in attention, awareness and emotion (1,2).
A key feature of mindfulness meditators may be the ability to recognise and accurately label emotions (3). Brain FMRI studies have shown more mindful people having increased ability to control emotional reactions in various areas associated with emotional regulation such as the amgydala, dlPFC, and ACC (4).
In a study (5) on the the effects of long term meditation on physical structure of the above brain regions, practitioners of mindful meditation who meditated 30-40 minutes a day, had increased thickness due to neuroplasticity of meditation in brain regions associated with attention and interoception (sensitivity to somatic or internal bodily stimuli) than the matched controls used in this study. Again the regions observed to have greater thickness via increased neural activity (neuroplasticity) were the PFC, right insula (interoception and this increased appreciation of bodily sensations and emotions) as well as the ACC in attention (and possible self awareness as ACC is also linked to consciousness) .
A structural MRI study (6) showed that experienced mindfulness meditators also had increased grey matter the right interior insula and PFC as well as, in unpublished data, in the hippocampus, which is implicated in memory but also in stress regulation. Thus mindfulness meditation and the fMRI and MRI studies show it is possible to train the mind to change brain morphology and functionality through the neuroplastic behaviour of meditating.
Brain regions consistently strengthen or which grow additonal “neural muscles” are those associated with emotional regulation and processing such as the dlPFC, ACC, insula and amgydala. Thus if we want, as recovering individuals, to shore up our early recovery, by strengthening the brain regions implicated in recovery success we meditate on a regular basis, daily, so that we can also improve those underlying difficulties in emotional regulation and processing.
By relieving emotional distress we greatly lessen the grip our condition has on us on a daily basis, We recover these functions. We will discuss the role of meditation on reducing emotional distress in later blogs.
References
1. Cahn, B. R., & Polich, J. (2006). Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychological bulletin, 132(2), 180.
2, Lutz, A., Slagter, H. A., Dunne, J. D., & Davidson, R. J. (2008). Attention regulation and monitoring in meditation. Trends in cognitive sciences, 12(4), 163-169.
3. Analayo. (2003). Satipatthana: The Direct Path to Awakening. Birmingham, UK: Windhorse Publications.
4. Creswell, J. D., Way, B. M., Eisenberger, N. I., & Lieberman, M. D. (2007). Neural correlates of dispositional mindfulness during affect labeling.Psychosomatic Medicine, 69(6), 560-565.
5. Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., … & Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. Neuroreport, 16(17), 1893.
6. Hölzel, B. K., Ott, U., Hempel, H., Hackl, A., Wolf, K., Stark, R., & Vaitl, D. (2007). Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neuroscience letters, 421(1), 16-21.
see also Hijacking the Brain
What recovers in Recovery? – Cognitive Control over emotions?
A core aspect of alcohol dependence is poor regulation of behavior and emotion.
Alcohol dependent individuals show an inability to manage the appropriate experience and expression of emotion (e.g., extremes in emotional responsiveness to social situations, negative affect, mood swings) (1,2). Dysfunctional emotion regulation has been considered a primary trigger for relapse (1,3) and has been associated with prefrontal dysfunction.
While current alcohol dependence is associated with exaggerated bottom-up (sub-cortical) and compromised top-down (prefrontal cortex) neural network functioning, there is evidence suggesting that abstinent individuals may have overcome these dysfunctional patterns of network functioning (4) .
Neuro-imaging studies showing chronic alcohol abuse to be associated with stress neuroadaptations in the medial prefrontal and anterior cingulate regions of the brain (5 ), which are strongly implicated in the self-regulation of emotion and behavioral self-control (6).
One study (2) looking at how emotional dysregulation related to relapse, showed compared with social drinkers, alcohol-dependent patients reported significant differences in emotional awareness and impulse control during week 1 of treatment. Significant improvements in awareness and clarity of emotion were observed following 5 weeks of protracted abstinence.
Another study (7) which did not look specifically at emotional regulation but rather on the recovering of prefrontal areas of the brain known to be involved also in the inhibition of impulsive behaviour and emotional regulation showed that differences between the short- and long-abstinence groups in the patterns of functional recruitment suggest different cognitive control demands at different stages in abstinence.
The long-term abstinent group (n=9) had not consumed cocaine for on average 69 weeks, the short-term abstinent (SA) group (n=9) had an average 0f 2.4 weeks.
Relative to controls, abstinent cocaine abusers have been shown to have reduced metabolism in left anterior cingulate cortex (ACC) and right dorsolateral prefrontal cortex (DLPFC), and greater activation in right ACC.
In this study the abstinent groups of cocaine addicts showed more elevated activity in the DLPFC ; a finding that has also been observed in abstinent marijuana users (8).
The elevation of frontal activity also appears to undergo a shift from the left to right hemisphere over the course of abstinence. Furthermore, the left inferior frontal gyrus (IFG) has recently been shown to be important for response inhibition (9) and in a task similar to that described here, older adults have been shown to rely more on left PFC (10). Activity observed in these regions is therefore likely to be response inhibition related.
The reliance of the SA group on this region suggests that early in abstinence users may adopt an alternative cognitive strategy in that they may recruit the LIFG in a manner akin to children and older adults to achieve behavioral results similar to the other groups.
Another study (11) noted the loss of grey matter in alcoholism that last from 6–9 months to more than a year or, in some reports, up to at least 6 years following abstinence (12 -14).
It has been suggested cocaine abuse blunts responses in regions important to emotional regulation (15)
Given that emotional reactivity has been implicated as a factor in vulnerability to drug abuse (16) this may be a preexisting factor that increased the likelihood of the development and prolonging of drug abuse
If addiction can be characterized as a loss of self-directed volitional control (17), then abstinence (recovery) and its maintenance may be characterized by a reassertion of these aspects of executive function (18) as cocaine use has been shown to reduce grey matter in brain regions critical to executive function, such as the anterior cingulate, lateral prefrontal, orbitofrontal and insular cortices (19-24) .
The group of abstinent cocaine addicts (11) reported here show elevations in (increased) grey matter in abstinence exceeded those of the healthy control in this study after 36 weeks, on average, of abstinence .
One possible explanation for this is that abstinence may require reassertion of cognitive control and behavior monitoring that is diminished during current cocaine dependence.
Reassertion of behavioral control may produce a expansion (25) in grey matter in regions such as the anterior insula, anterior cingulate, cerebellum, and dorsolateral prefrontal cortex .
All brain regions implicated in the processing and regulating of emotion.
References
1. Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive-behavioral therapy for alcohol dependence. J Consult Clin Psychol. 2011;79:307–318.
2. Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Alcohol Clin Exp Res. 2008;33:388–394.
3..Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990
4. Camchong, J., Stenger, A., & Fein, G. (2013). Resting‐State Synchrony in Long‐Term Abstinent Alcoholics. Alcoholism: Clinical and Experimental Research, 37(1), 75-85.
5. Sinha, R., & Li, C. S. (2007). Imaging stress- and cue-induced drug and alcohol craving: Association with relapse and clinical
implications. Drug and Alcohol Review, 26(1), 25−31.
6. Beauregard, M., Lévesque, J., & Bourgouin, P. (2001). Neural correlates of conscious self-regulation of emotion. Journal of
Neuroscience, 21(18), RC165
7. Connolly, C. G., Foxe, J. J., Nierenberg, J., Shpaner, M., & Garavan, H. (2012). The neurobiology of cognitive control in successful cocaine abstinence. Drug and alcohol dependence, 121(1), 45-53.
8. Tapert SF, Schweinsburg AD, Drummond SP, Paulus MP, Brown SA, Yang TT, Frank LR. Functional MRI of inhibitory processing in abstinent adolescent marijuana users.Psychopharmacology (Berl.) 2007;194:173–183.[PMC free article]
9. Swick D, Ashley V, Turken AU. Left inferior frontal gyrus is critical for response inhibition. BMC Neurosci. 2008;9:102.[PMC free article]
10. Garavan H, Hester R, Murphy K, Fassbender C, Kelly C. Individual differences in the functional neuroanatomy of inhibitory control. Brain Res. 2006;1105:130–142
11. Connolly, C. G., Bell, R. P., Foxe, J. J., & Garavan, H. (2013). Dissociated grey matter changes with prolonged addiction and extended abstinence in cocaine users. PloS one, 8(3), e59645.
12. Chanraud S, Pitel A-L, Rohlfing T, Pfefferbaum A, Sullivan EV (2010) Dual Tasking and Working Memory in Alcoholism: Relation to Frontocerebellar Circuitry. Neuropsychopharmacol 35: 1868–1878 doi:10.1038/npp.2010.56.
13. Wobrock T, Falkai P, Schneider-Axmann T, Frommann N, Woelwer W, et al. (2009) Effects of abstinence on brain morphology in alcoholism. Eur Arch Psy Clin N 259: 143–150 doi:10.1007/s00406-008-0846-3.
14. Makris N, Oscar-Berman M, Jaffin SK, Hodge SM, Kennedy DN, et al. (2008) Decreased volume of the brain reward system in alcoholism. Biol Psychiatry 64: 192–202 doi:10.1016/j.biopsych.2008.01.018.
15, Bolla K, Ernst M, Kiehl K, Mouratidis M, Eldreth D, et al. (2004) Prefrontal cortical dysfunction in abstinent cocaine abusers. J Neuropsychiatry Clin Neurosci 16: 456–464 doi:10.1176/appi.neuropsych.16.4.456.
16. Piazza PV, Maccari S, Deminière JM, Le Moal M, Mormède P, et al. (1991) Corticosterone levels determine individual vulnerability to amphetamine self-administration. Proc Natl Acad Sci USA 88: 2088–2092. doi: 10.1073/pnas.88.6.2088
17. Goldstein RZ, Volkow ND (2002) Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry 159: 1642–1652. doi: 10.1176/appi.ajp.159.10.1642
18. Connolly CG, Foxe JJ, Nierenberg J, Shpaner M, Garavan H (2012) The neurobiology of cognitive control in successful cocaine abstinence. Drug Alcohol Depend 121: 45–53 doi:10.1016/j.drugalcdep.2011.08.007.
19. Liu X, Matochik JA, Cadet JL, London ED (1998) Smaller volume of prefrontal lobe in polysubstance abusers: a magnetic resonance imaging study. Neuropsychopharmacol 18: 243–252 doi:10.1016/S0893-133X(97)00143-7.
20. Bartzokis G, Beckson M, Lu P, Nuechterlein K, Edwards N, et al. (2001) Age-related changes in frontal and temporal lobe volumes in men – A magnetic resonance imaging study. Arch Gen Psychiatry 58: 461–465. doi: 10.1001/archpsyc.58.5.461
21. Franklin TR, Acton PD, Maldjian JA, Gray JD, Croft JR, et al. (2002) Decreased gray matter concentration in the insular, orbitofrontal, cingulate, and temporal cortices of cocaine patients. Biol Psychiatry 51: 134–142. doi: 10.1016/s0006-3223(01)01269-0
22. Matochik JA, London ED, Eldreth DA, Cadet J-L, Bolla KI (2003) Frontal cortical tissue composition in abstinent cocaine abusers: a magnetic resonance imaging study. NeuroImage 19: 1095–1102. doi: 10.1016/s1053-8119(03)00244-1
23. Lim KO, Wozniak JR, Mueller BA, Franc DT, Specker SM, et al. (2008) Brain macrostructural and microstructural abnormalities in cocaine dependence. Drug Alcohol Depend 92: 164–172 doi:10.1016/j.drugalcdep.2007.07.019.
24. Ersche KD, Barnes A, Jones PS, Morein-Zamir S, Robbins TW, et al. (2011) Abnormal structure of frontostriatal brain systems is associated with aspects of impulsivity and compulsivity in cocaine dependence. Brain 134: 2013–2024 doi:10.1093/brain/awr138.
25. Ilg R, Wohlschlaeger AM, Gaser C, Liebau Y, Dauner R, et al. (2008) Gray matter increase induced by practice correlates with task-specific activation: A combined functional and morphometric magnetic resonance Imaging study. J Neurosci 28: 4210–4215 doi:10.1523/JNEUROSCI.5722-07.2008.
The Distress at the Heart of Addiction and Alcoholism
This blog is written for alcoholics and those who love and live with them, by alcoholics in recovery. For those who know what it is like to live with alcoholism but would also like to know why alcoholism affects the alcoholic and those around him in the way it does.
We write this blog to help us and you understand how the alcoholic brain works; why they do the things the do, why they act the way they do. Why is it everything is going great and suddenly the alcoholic in your life “flies off the handle’ and acts in an emotionally immature way, which can often cause hurt to others around them? What is the reason behind this “Jekyll and Hide” emotional responding?
Why do they suddenly cut off their emotions so profoundly it leaves your emotions in limbo, confused and upset?
In this blog we seek to explain, as researchers, in terms of the processes of the brain, why alcoholics, particularly those in recovery, do the things the way they do, act the way they do.
We hope to explain this disease state, which alcoholics themselves call a “emotional disease’, a “cancer of the emotions’, a “parasite that feeds on the emotions” or quite simply “a fear based illness”. It appears that alcoholics in recovery are aware to a large extent of what they suffer from. But why do they do what they do sometimes if they know what is going on? Why do they not seem to be able to help themselves from engaging in certain responses and behaviours?
Why do they endless engage in self defeating resentments, taking “other peoples’ inventory” or criticizing, why do they project into future scenarios and then get emotionally paralyzed by doing so, why do they run through the list of cognitive distortions on a daily basis, why do they get self absorbed and engage in “me, me, me” behaviour!? Why do they indulge in self pity to the extent they end up in full blown depression?
More importantly, perhaps, how do various therapeutic strategies deal with these behaviours and seek to challenge and address them? And do these therapies, in time through practice and the neuroplasticity (neural reshaping of the brain via behaviour) change how they act, feel and live in this life. In short, how does recovery change the brains of alcoholics for the better?
As we are personally well aware, self knowledge does not bring recovery – only action does. But this action can be based solidly on a better understanding of what goes on in the brain of an alcoholic for example, why should I mediate? What beneficial, adaptive change will that bring, how will that “help me recover”? What is the point of doing the steps, how exactly do they effect change in one’s alcoholic brain? Is there a good healthy neurobiological reason for going to mutual aid group meetings like AA or SMART?
We also believe that academic research definitions of alcoholism are inadequate – the latest DSM V equates the emotional difficulties we highlight here as ‘co-morbidities’, conditions that occur alongside the condition of alcoholism. We disagree, we suggest these ‘co-morbidities’ (co-occurring psychiatric disorders) are a main reason why we become alcoholics, they are what make us vulnerable, along with genes and environment to becoming alcoholic.
Most alcoholics feel they never fitted in, were emotionally hyper “sensitive”, engaged in risky behaviours, got into trouble without intending to, and other impulsive behaviours which we believe are illustrative of an emotional dysregulation which makes certain individuals vulnerable to becoming alcoholic.
Science tells us there are many such vulnerabilities in children of alcoholics. The alcohol regulated, medicated these errant emotions which caused such distress, even at an early age. It is these emotional processing deficits and emotional dysregualtion (i.e. poor control of emotions, especially when distressed!) which lie at the heart of the this psychopathology or if you like this psychiatric disorder called alcoholism.
It is a distress-based condition, day in day out, and we formally believe that various therapeutic regimes like the 12 steps, DBT, ACT or CBT, etc all treat this inherent distress state in some way. It is this distress state that activates this “fear-based illness”, that makes one hyper aware of cues, alcohol, it is this distress that provokes memories of drinking, alcohol use schemata, that trains one attention on people places and things from the past. Without this distress our illness barely gets activated!
For example, does your loved alcoholic, “over do things”on a regular basis, do they engage in short term thinking, or “quick fix ” thinking. Do they resist your attempts at sensible long term , goal directed, “thought through thinking”?
Does your alcoholic work himself to a frazzle, do they easily become exhausted by overdoing it, whatever it is? Do they have a series of new addictions? Are they perfectionist doing too much, or nothing anything at all? Perfectionism is distress based.
Does your alcoholic fear the future, but continually project their thinking into the future? Do they have an intolerance of uncertainty, do they endless ruminate about things, do they react rather than act? Do the most simple decisions provoke a “fight or flight” response? Do they frequently come up with “I know how to do this, I have a great idea!” Only for it to be the opposite of a great idea! Do they give people “rent free room in their heads” because of resentments – replying the same old tape in their minds, over and over and over again? All distress based?
“Fear based” is distress based.
A recent study showed that alcoholics have a part of the brain that helps process emotions but it doesn’t work properly so is overactive all the time; it is exhausting being on red alert, all the time , living on a state of emergency. Hence step 11 in the the 12 steps.
The problem with this hyperactive brain region, called the ventromedial prefrontal cortex, is that it also cuts out , hypo-activates, when more or excessive stress is applied and another compulsive area of the brain, the basal ganglia, takes over. This part is automatic, habitualized, automatic, compulsive! It results in more more more, and is driven by distress not goal directed consideration. It simple does, does, does, without consideration of future consequence. Sound familiar??
How did your loved alcoholic get to be this way? What happened to your own alcoholic brain? We believe there is a vulnerability to these aforementioned emotional difficulties as certain brain areas which regulate emotion not working properly. This means they are smaller, impaired and do not function optimally or are not connected properly.
Do you know an alcoholic who does not accurately know how he is feeling properly, does not know what emotion he is experiencing? Cannot label to emotion properly which makes processing of it difficult? Can’t rely on a neural feedback to tell himself when he is tired, angry, hungry and that he should HALT? This is the insular cortex not working properly.
Does your alcoholic see error everywhere (and worse still give a running commentary on it!?), always whinging about that not being right, or that being wrong. Why can’t they do things properly, be more perfect!! That is partly to do with impairment of the anterior cingulate cortex which monitors error in the environment.
This fear based stuff? That is a hyperactive amgydala, the “anxious amgydala”, and it also acts as a switch between memory systems, from explicit to implicit memory, and recruits the compulsive “go,go, go” area of the dorsal striatum from the always “on the go”, hyperactive, ventromedial cortex.
The amgydala is at the heart of alcoholism and addiction. It not only switches memory but also reward/motivation/ and emotional response so that distress provokes a habitualised “fight or flight response” in the dorsal striatum.
It is said that alcoholics are emotional thinkers, but this region is also an emotional “do” area which means emotional distress acts as a stimulus response. The brain responds to the stimulus of distress in other words. As addiction and alcoholism progress the ways addicts and alcoholics react become limited in line with addiction severity. The further the alcoholic gets in alcoholism the more he will react out of distress, the more automatic his behaviours become, the more short term his decision making will be, the more he has to fight automatic urges and automatic drink-related thoughts, the more he has to contend with “fight or flight” thinking and feeling.
Add to this a brain that is out of balance, does not have homeostasis, natural neurochemical balance, but has a state called allostasis, where the brain constantly attempts to finding stability via constant change, and the fact that the alcoholic brain has too much Glutamate, an excitatory neurotransmitter, the “go neurochemical”, and not enough GABA, an inhibitory neurotransmitter, the brains’ natural brakes”, (and which is increased by drinking alcohol) the stop or slow down chemical and that this also helps slow down an abnormal heart rate variability (HRV) found in alcoholics.
Alcoholics have a different heart rate variability meaning we have a heart rate more suited to being ready for the next (imagined) emergency. The effects of alcohol are thus more profound on this group, and this HRV is also seen in children of alcoholics so represents a profound vulnerability to later alcoholism.
Add to that depleted levels of of dopamine, which is very important in the addiction cycle. The problem with dopamine supplies is that our excessive levels of stress reduce our amount of dopamine, that we are always on the look out for more dopamine. Add to this that stressful states increase our brain in “dopamine seeking” in an attempt at transient allostasis and you have a brain that is always trying to get a buzz out of something, especially when in distress states.
Then there is other deficits to the serotonin system, to the natural opioids system, to oxytocin, all of which take a beating and are reduced by excessive stress systems. But all are increased via love and looking out for our fellow man, our families, loved ones and other’s in recovery. We can manipulate our brain chemistries, this is what happens in recovery in fact!
Too much stress on the brain spreads like a forest fire throughout the brain, lowering levels of essential neurotransmitters, impairing memory and turning one from a goal directed action to a compulsive reaction type of guy. The alcoholic brain is always primed to go off!!
Chronic stress also impairs the prefrontal cortex, the cognitive, conscious “top down” controller of the brain’s emotions and urges, instincts and so on. It doesn’t help that it doesn’t work too well in alcoholics. The brain of an alcoholic is a “spillover” brain, it is a brain that spills over into various types of disinhibition, impulsivity and compulsivity . It often acts before considering, speaks before thinking. decides this is a great idea with out consulting, reacts without sufficient reason or cause.
It needs help, this alcoholic brain. From another brain, from someone other than himself.
Recovering alcoholics need an external prefrontal cortex to help with the top down cognitive control of the subcortical emotional and motivational states. The problem with emotions are they, in the alcoholic brain, have become entwined with reward. We feel a certain way, negative for example, and fix this negative feeling, with something rewarding, makes us feel better, more positive, less self reflective, and it seems this has been the case with certain alcoholics since childhood. Dealing with emotions by the granting of treats.
Feeling better by consuming. Fixing feelings via external substances. Sub contracting our emotional regulation. Finding different feelings in a bottle, or a pill, or a syringe or snorting them up one’s nose. Alcoholics need a spiritual awakening, a psychic change, a change in consciousness, in self schema; this sudden change in how we feel about the world (including memories of our past life) because the old feeling about the world will lead to the sane old behaviours. Plus alcohol and drugs were crude approximates of this change in consciousness, this spirit awakenings, they dramatically and very instantaneously helped change our feelings, thoughts, perceptions about the world around us. They helped us fit in.
This is the purpose of a spiritual awakening too, a sudden change of consciousness. We believe the best and most sudden way to achieve this is to let go of the thing that causes all the suffering in the first place, the self. It appears we can live without the “self” . It also appears helping others brings a bigger buzz than even helping ourselves.
Helping others reduces our distress. and many many other therapeutic benefits to brain chemistry. This brain also needs some one outside of self, outside the self regulation network in the brain which is so impaired and cannot be relied on because at times it is maladaptive. Can’t be counted on the make the right decision because it favours short term over the long term, is based on “fight or flight “thinking and rational, hence is distorted by fear.
If we have been thinking in this maladaptive way all our lives it is no wonder we ended up where we have. We used alcohol to deal with our errant and quite frightening emotions. I positively ran away from my own emotions.
I used to say to my wife, the main reason for my drinking is “to get away from my self”. Now we have to find a solution to living with oneself, these sometimes torturous alien state of emotional sobriety.
I remember being asked by a counsellor to sit with my emotions for half on a hour. I felt I was being possessed by some poltergeist, the feelings associated with emotional regulation were so alien to me, so frightening. I didn’t know what they were even. I had to have by wife label them for me and help me process them.
I believe steps 4 and of 12 step programs help one emotional regulation hundreds and hundreds of unresolved, unprocessed emotions from the past otherwise they will continue to be in there, haunting us like “neural ghosts” from the past, adding emotional distress to our conscious daily experience and encouraging relapse. This is the case for many newly recovering alcoholics. Being haunted by a million thoughts produced by rampant emotional dysregulation.
Resentments swirling around the mind and driving the newcomer back to relapse. What the newcomer finds is that the drink stops working, and the emotional difficulties remain, in fact much worsened by years and years of sticking a neurotoxin down our throats and in into our brains. Havoc is then further reaped on an already not fully functioning brain.
In AA they often they say that they are stuck at the emotional age of when they started drinking which is usually around the early teens when the cognitive part of the brain that controls emotions is still developing. But we act much more immaturely than that, we act like the terrible twos or children. Our emotional brains never really grew up. This emotional dysregulation apparent as teens then shaped all our future decisions and eventually our alcoholism. That is what they mean in AA, when they say all your best thinking got you here. So there you have it . Sound familiar? Recognize anyone here?