In early recovery I was amazed that some people in recovery said they never thought about alcohol after a few weeks into recovery. Or rather than thoughts related to alcohol rarely drifted across their minds.
I was alarmed by this as thoughts of alcohol rarely left my mind in early recovery.
They came to me rather than me actively going to retrieve thoughts about alcohol myself, consciously or deliberately.
I now realise that this was due to two main reasons.
First of all, fear of drinking is a distress which activates thoughts of alcohol as distress and negative emotions (and negative self perception/schema) seem to automatically retrieve thoughts of alcohol as there has been some habitual fusion of negative emotion with urge to drink in the alcoholic brain.
This is because my alcoholism resulted in compulsive drinking, i.e. my drinking was mainly to do with relieving distress, and that is what compulsion is, automatic behaviours that relieve distress.
Secondly and tied to this point, is that this compulsive drinking in itself is also linked to how chronic my drinking became.
I was completely addicted to alcohol at the end of my drinking so my alcoholism is very chronic.
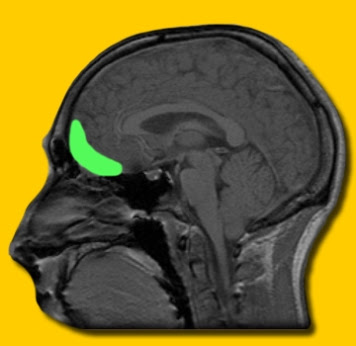
In terms of neuroscience this means any distress activates a motoric part of my brain, the dorsal striatum, a part of the brain that deals with stimulus response or automatic response the internal stimulus of distress, which activates an automatic approach or preparation of movement towards getting a drink.
This is expressed in terms of instruction in the brain as automatically occurring intrusive thoughts about drinking alcohol. This is also called an alcohol use schema because as a schema it is procedural way to deal with distress, i.e. have distress automatically deal with it by drinking.
I still find it fascinating that even automatic behaviours have thoughts that accompany them. Although nothing is completely automatic and we have a brief period of time in which to react or not.
By not reacting or acting on this thoughts they appear to lessen in intensity. The more we do not react the less intense these thoughts become. Finding new ways to cope with distress lessens their grip on us too and eventually they practically disappear.
I have found I have to be very very distressed in recovery for thoughts of alcohol to come revisiting my mind.
This involuntary retrieval of drug related thoughts is thus a hallmark of addicted populations as it happens automatically, implicitly without you having to consciously and explicitly retrieve these thoughts and associated images from your memory banks. They just pop up without your permission.
The intensity of obsessive thoughts about alcohol is said to predict relapse rates (1), with addicts motivated to use drugs to “silence” obsessive thoughts (2).
The idea that abstinence automatically decreases alcohol-related thoughts is challenged by research (3) and supported by clinical observation that among abstinent alcohol abusers, alcohol-related thoughts and intrusions are the rule rather than exception (4).
Modell and colleagues (1992) highlighted symptomatic similarities between addiction and obsessive compulsive disorder with subjective craving for drugs or alcohol characterized as having obsessive elements. (eg, the compulsive drive to consume alcohol, recurrent and persistent thoughts about alcohol, and the struggle to control these drives and thoughts) similar to the thought patterns and behaviours of patients with obsessive-compulsive illness (5).
Modell et al. also point to the potential similarities in underlying neural pathways implicated in the two disorders, suggesting that they may share a similar aetiology.
The Obsessive Compulsive Drinking Scale (OCDS) implies that as the severity of this illness progresses, so does the intensity of the obsessive thoughts about alcohol and the compulsive behaviours to use alcohol.
Kranzler et al. (1999) showed relapsers who scored higher in ‘obsessions’ craving measured by the OCDS predicted relapse in the 12 months after treatment completion (6).
This may also be a reflection of addiction severity too! As addicts and alcoholics become more addictive brain imaging shows a shift in “reward processing” from the ventral striatum to the dorsal striatum.
The DS as stated above is in charge of more automatic, compulsive reaction.
This shift from VS to DS may also be marked by an increased emergence of automatic thoughts, which the authors also suggested as the cognitive thoughts and images of automatized drug action schemata (2).
In fact, this is demonstrated by correlations indicating that dorsal striatum activation is lowest in participants with low OCDS scores. And vice versa, highers OCDS scores with increased DS activation.
This means, in simple terms, that more severe addiction may be associated with more intrusive/obsessive thoughts and less severe with less thoughts.
So if you are in a meeting or in other treatment environments and someone in recovery says they never have any obsessive thoughts or intrusive thoughts consider the possibility that their addiction did not become as severe as your addiction?
Either way these thoughts are not your own but the automatic thoughts of addiction so be careful not to react to them.
They are frightening at first, but gradually becoming irritating and annoying before occurring less and less as recovery and your non reaction progress.
If you learn to habitually not to react emotionally to them they start to lose their grip and become less severely intrusive.
Most days I do not have any intrusive thoughts. This is because my recovery has progressed.
In many ways, recovery usually goes in the opposite direction to addiction.
References
1.. Bottlender, M., & Soyka, M. (2004). Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol and Alcoholism, 39(4), 357-361.
2. 6. Tiffany, S. T. (1990). A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological review, 97(2), 147.
3. Caetano, R. (1985). Alcohol dependence and the need to drink: A compulsion? Psychological Medicine,
15(3), 463–469.
4. Hoyer, J., Hacker, J., & Lindenmeyer, J. (2007). Metacognition in alcohol abusers: How are alcohol-related intrusions appraised?. Cognitive Therapy and Research, 31(6), 817-831.
5. Modell, J. G., Glaser, F. B., Mountz, J. M., Schmaltz, S., & Cyr, L. (1992). Obsessive and compulsive characteristics of alcohol abuse and dependence: Quantification by a newly developed questionnaire.
Alcoholism: Clinical and Experimental Research, 16, 266-271.
6. Kranzler, H. R., Mulgrew, C. L., Modesto-Lowe, V. and Burleson, J. A.
(1999) Validity of the obsessive compulsive drinking scale (OCDS): Does craving predict drinking behavior? Alcoholism: Clinical and Experimental Research 23, 108–114.
7. Vollstädt‐Klein, S., Wichert, S., Rabinstein, J., Bühler, M., Klein, O., Ende, G., … & Mann, K. (2010). Initial, habitual and compulsive alcohol use is characterized by a shift of cue processing from ventral to dorsal striatum.Addiction, 105(10), 1741-1749.