“Mindfulness Training Ameliorates Addiction by Targeting Neurocognitive Mechanisms
ATTENTIONAL BIAS
Given that drug-use action schemas may be evoked by cues associated with past substance use episodes, activation of addictive habits may be interrupted by re-orienting attention from substance-related stimuli to neutral or salutary objects and events. MBIs may be especially efficacious in that regard. Focused attention and open monitoring mindfulness practices capitalize on attentional orienting, alerting, and conflict monitoring – the fundamental components of attentional control (89, 90). Consequently, studies indicate that mindfulness is linked with enhanced attention regulation (61, 91). For instance, mindfulness training is associated with strengthening of functional connectivity within a dorsal attentional network (92) and MBIs can increase attentional re-orienting capacity, i.e., the ability to engage, disengage, and shift attention efficiently from one object to another subserved by dorsal attentional systems (93, 94). Other studies demonstrate that long-term mindfulness training strengthens alerting (93,95), i.e., a vigilant preparedness to detect and attend to incoming stimuli, subserved by the ventral attentional stream. In addition, dispositional mindfulness is positively associated with self-reported attentional control (68) and behavioral indices of sustained attention capacity (70). Recently, data from a randomized controlled trial indicated that 8 weeks of Mindfulness-Oriented Recovery Enhancement led to significant reductions in attentional bias to pain-related cues in a sample of opioid-misusing chronic pain patients (96).
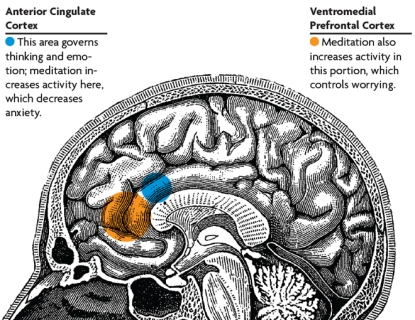
MBIs may target addiction attentional bias by facilitating attentional disengagement from substance-related stimuli. In support of this hypothesis, a study of alcohol dependent adults in residential treatment identified a significant negative correlation between dispositional mindfulness and alcohol attentional bias for stimuli presented for 2000 ms that remained robust even after controlling for alcohol dependence severity, craving, and perceived stress (1). Hypothetically, alcohol dependent persons higher in dispositional mindfulness might exhibit increased capacity for attentional disengagement from alcohol cues by virtue of enhanced PFC and anterior cingulate cortex functionality, as these brain structures have been implicated in addiction attentional bias (97–99). Concomitantly, the degree to which alcohol dependent individuals higher in dispositional mindfulness were better able to disengage their attention from alcohol cues than their less mindful counterparts predicted the extent of heart-rate variability (HRV) recovery (an index of prefrontal-autonomic regulation) from stress-primed alcohol cue-exposure (67). Mindfulness training may also affect attentional orienting to substance-related cues. Among a sample of alcohol dependent adults in inpatient treatment, Mindfulness-Oriented Recovery Enhancement was found to result in significant effects on alcohol attentional bias for cues presented for 200 ms (7), indicating modulation of automatic initial orienting to alcohol cues [c.f. (23)]. In individual difference analyses, reductions in attentional bias following Mindfulness-Oriented Recovery Enhancement were significantly associated with decreases in thought suppression, which were, in turn, correlated with increases in HRV recovery from alcohol cue-exposure and improvements in self-reported ability to regulate alcohol urges.
Hence, mindfulness training may strengthen the capacity to regulate attention in the face of conditioned stimuli associated with past substance use, countering attentional biases by refocusing attention on neutral or health-promoting stimuli (e.g., the sensation of one’s own breath or a beautiful sunset). Repeatedly redirecting attention from substance-related cues toward innocuous stimuli may foster extinction of associations between substance-related cues and drug-use action schema. This potential mechanism may explain how attentional bias modification among addicts leads to decreased substance use and improved treatment outcomes (100,101). Future research could evaluate the effects of mindfulness training and MBIs on addiction attentional bias with the use of a dot probe task alone or coupled with eye tracking and analysis of event-related potentials (ERPs) to determine at what stage of attentional selection (initial orienting vs. later attentional disengagement) training has significant effects.
CUE-ELICITED CRAVING
The urge to seek intoxication from addictive substances is driven, in part, by reactivity to substance-related stimuli which have been conferred incentive salience, and is magnified by negative affective states. Several studies demonstrate that MBIs can produce significant reductions in craving (4,8,102–105). However, other studies have failed to identify significant reductions in craving among participants of MBIs (7, 106–108).
Mindfulness-based interventions may positively influence craving-related processes in several ways. First, mindfulness training may decrease bottom-up reactivity to drug-related stimuli, as mediated by reduced activation in the subgenual anterior cingulate cortex and striatum during exposure to substance cues (105). Second, mindfulness training may decouple negative emotion from craving. Although negative emotion is a common precipitant of craving and subsequent relapse (109), mindfulness training may extinguish this association, such that an addict experiencing sadness, fear, or anger could allow these emotions to arise and pass without triggering an appetitive reaction. Indeed, substance dependent individuals participating in Mindfulness-Based Relapse Prevention were less likely to experience craving in response to depressed mood, and this reduced craving and reactivity to negative emotion predicted fewer days of substance use (110).
MBIs may also produce therapeutic effects by increasing awareness of implicit craving responses. Tiffany (20) proposed that conscious craving occurs when an activated drug-use action schema is blocked from obtaining the goal of drug consumption. As such, persons in acute withdrawal, persons unable to obtain drugs (e.g., due to lack of funds or availability), or persons attempting to maintain abstinence in the face of triggers may experience an upwelling of craving for substances. In contrast, according to this theory, addicts who are able to obtain and use drugs in an unimpeded fashion would not experience craving. Similarly, persons in long-term residential treatment who are isolated from drug-related cues are unlikely to be conscious of craving. Without awareness of craving, the addict may unwittingly remain in high-risk situations and thus be especially subject to relapse. Indeed, lack of awareness of substance craving has been shown to be predictive of future relapse (111). MBIs may increase conscious access to the appetitive drive to use substances by virtue of their effects on increasing interoceptive awareness (78, 112). In that regard, mindfulness training has been shown to increase activity in the anterior insula during provocations by emotionally salient stimuli (113, 114). The anterior insula subserves interoception and awareness of the physical condition of the body, among other related processes (115). Increased neural activity in the insula during mindfulness meditation may index heightened access to interoceptive information.
In synthesizing the findings regarding attentional bias and cue-induced craving, we suggest that MBIs may restructure attentional bias away from drug-related reinforcing stimuli (e.g., drug-cues, negative affective stimuli) and facilitate the addict’s attempts to deal with associated cravings. We posit that mindfulness-centered regulation of cue-elicited appetitive responses occurs as a result of strengthening frontal-executive circuit-function and enhancing neural communication to the hippocampus and thalamus through formal and informal mindfulness meditation practices. The hippocampus is critical for context-dependent learning and memory – with reciprocal connectivity to brain regions that code for reward (ventral striatum), interoception (insula), affect (amygdala), and thalamus. In turn, the thalamus, a complex structure that is generally considered to serve as a relay station between limbic, striatal, and cortical circuits, contains efferent and afferent projections with striatal, limbic, somatosensory, ACC, lateral and medial PFC, and OFC. Thus, the recovering addict may utilize mindfulness training to become aware of which cues are under the spotlight of attention, and become more sensitive to how those cues may trigger changes in body state and motivation drive.
Hence, mindfulness may increase awareness of craving and thereby facilitate cognitive control of otherwise automatic appetitive impulses. In that regard, a recent study found that participation in Mindfulness-Oriented Recovery Enhancement was associated with decreased correlation strength between opioid craving and opioid misuse, suggesting that mindfulness training may have decoupled appetitive responses from addictive behaviors (8). This mechanism may explain the disparate findings vis-a-vis the effects of mindfulness on craving: because of potential underreporting of baseline levels of craving among individuals with impaired insight into their addiction (34), this increased awareness may confound researchers’ attempts to measure the impact of mindfulness training on craving, resulting in an apparent lack of change in craving over time.
The effects of mindfulness on cognitive regulation of craving might be measured by utilizing neuroimaging methodology (e.g., fMRI) to investigate neural circuitry function while participants attempt to regulate their craving response to salient drug-cues. For example, cognitive regulation appears to decrease cigarette craving concomitant with increased activity in dACC (116) and prefrontal regions coupled with attenuated activity in striatal regions (117). A complementary approach to probing the effects of mindfulness on regulating craving may be to utilize real-time fMRI (rt-fMRI). rt-FMRI involves providing subjects with real-time feedback of the BOLD signal within a brain region of interest (ROI) while they attempt to regulate the response within that ROI. This approach has been used to manage pain (118) and reduce cigarette cue craving in nicotine dependent smokers during smoking cessation (119). Evaluating the effects of mindfulness-centered regulation of craving-related neural circuitry in real-time may include a number of benefits including: (a) directly measuring which circuits are being effectively modulated and which are not; (b) feedback to the subject that will help guide mindfulness efforts; and (c) identifying individual differences associated with differential effects of MBIs on specific neural mechanisms.
COGNITIVE APPRAISAL
Insofar as stress evokes automatic responses and impairs prefrontally mediated cognitive control functions (120), exposure to socioenvironmental stressors may render addicts in recovery vulnerable to relapse (1, 22, 121). Mindfulness training may allay stress-induced relapse by virtue of its stress-reductive effects (122). Although early theorists believed that mindfulness meditation reduced stress primarily by evoking a generalized relaxation response (123), modern research indicates that mindfulness practice may also attenuate stress by targeting cognitive mechanisms (1, 124). One potential target of mindfulness is cognitive appraisal, the process whereby stimuli and their environmental context are evaluated for their significance to the self (125). Appraisals of threat or harm elicit negative emotional reactions coupled with activation of stress physiology. When recurrent, such emotional reactivity biases perception, leading to exaggerated, overestimated appraisals of threat and underestimations of self-efficacy (126), and ultimately, sensitization to future stressors (127).
In contrast, mindfulness, which has been conceptualized as a non-reactive form of awareness (128) may enable the individual to cognitively appraise his or her present circumstances with less emotional bias, and to more accurately assess his or her ability to cope with present challenges (60). Thus, MBIs may impact both primary (rapid and implicit) and secondary (slow and explicit) appraisal processes (125). In partial support of this hypothesis, a recent neuroimaging study revealed that, in contrast to a meditation-naive control group, mindfulness meditation practitioners exhibited decreased reactivity to briefly presented negative emotional cues in frontal-executive brain regions (i.e., dorsolateral PFC) and less deterioration of positive affect in response to cue-elicited amygdala activation (31). These data suggest that mindfulness training may alter the allocation of cognitive resources during appraisal of negative emotional stimuli and attenuate the influence of limbic reactivity on mood state. Other research demonstrates that mindfulness training minimizes emotional interference from unpleasant stimuli [e.g., Ref. (129)]. In so doing, mindfulness training may reduce biases toward negative emotional information processing. Among persons with a history of depression, Mindfulness-Based Cognitive Therapy reduces overgeneral memories (130) and cognitive bias toward negative information (131). Among individuals suffering from chronic pain, Mindfulness-Oriented Recovery Enhancement decreases cognitive bias toward pain-related cues (96). Together, these findings suggest that MBIs may decrease negative emotional bias in initial cognitive appraisal processes, thereby reducing the downstream effects of stress on addictive behavior. As mindfulness-centered regulation enhances cortico-thalamic-limbic functional connectivity, the recovering addict becomes more aware of relations between attention, emotional state, and motivation. This awareness provides an opportunity to deploy cognitive strategies to respond to the environment in a more adaptable context-dependent manner, rather than responding from a pattern of overlearned reactive behaviors.
References
1. Garland, E. L., Froeliger, B., & Howard, M. O. (2013). Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Frontiers in psychiatry, 4.